
New Zealand’s National Cot Death Prevention Programme
The initiative
The results of a major scientific study (the New Zealand Cot Death Study, conducted over three years from 1987) were used to develop a prevention programme to reduce infant mortality rates. The study had found that there were “three risk factors that are potentially amenable to modification: prone sleeping position of the infant, maternal smoking and lack of breastfeeding.” [2] These risk factors were thought to account for 79 percent of deaths from SIDS.
The government initiated the National Cot Death Prevention Programme in 1991 with the overall aim to reduce the total SIDS rate from 2.5 per 1,000 live births in 1991 to 1.0 per 1,000 by 2000. Additionally they wanted to reduce the Maori SIDS rate from 6.9 to 2.5 per 1,000 live births by 2000. They aimed to do this by three specific objectives:
- To reduce the number of pregnant mothers smoking from 33% in 1991 to 25% of less by 1997 and to less than 20% by 2000.
- “To increase exclusive breastfeeding rates at three months from 60% in 1995 to 70% by 1997 and 75% by 2000.
- To maintain the side and back sleep positions for infants at six weeks at the 1991 prevalence rate of 95%. [3]
The programme was developed and rolled out in four phases: preparation; informing health professionals; informing the public (through public awareness programmes in the media and communities) and parents (by promoting parent knowledge and healthy behaviour); and maintenance and supportive activities.
The challenge
In New Zealand in the 1980s, “one in every 250 babies died suddenly, unexpectedly and without explanation.” [1] a higher incidence of Sudden Infant Death Syndrome (SIDS) than had been observed in other developed countries. In 1986, it accounted for 65 percent of deaths among babies. Naturally, reducing the incidence of SIDS, or cot death, became a national priority.The public impact
The programme had an almost immediate impact on the incidence of cot death:
- “The fall in SIDS mortality was dramatic, with a halving of the SIDS mortality rate, within 2 years and this was accompanied by a reduction in total (all causes) postneonatal mortality (1-11 month mortality) showing that the reduction was real. [4]
- “Mortality rates have continued to decline, albeit more gradually and this has been attributed to the reduction in the prevalence of side sleeping position.”
Stakeholder engagement
There were a large number of stakeholders in this programme, all of whom were strongly engaged:
- The New Zealand Department of Health and district health boards (DHBs) promoted and part-funded the programme.
- The Hawke's Bay Medical Research Foundation, an independent funding body, demonstrated its engagement by funding the salary of the programme coordinator.
- The New Zealand Cot Death Association.
- Health practitioners demonstrated their engagement by passing on the message, as did Kohanga Reo teachers.
- Plunket, an independent foundation, demonstrated engagement through its nurses, who visit 90 percent of infants in New Zealand. “[Plunket nurses] spread information to parents and reinforced the key messages by putting prevention stickers on the infant record books which are given routinely to all parents of newborn infants. If parents smoked, the nurses reinforced the ‘don't smoke' messages.” [5]
- “Community groups engaged by attending discussion groups and by developing locally-specific campaign materials to add to the government's materials.”
Political commitment
The government of New Zealand and DHBs demonstrated their commitment in three key ways:
- Policy commitment - “the three messages have been included in the priorities for child health in New Zealand and in the recently released service statement for area health board child health services” [6].
- Legislative commitment - the government passed the Smoke-free Environments Act 1990, which contributed to one of the objectives of the programme.
- Economic commitment -the Department of Health funded the development of the Baby Health Care Programme and a number of public awareness initiatives.
Public confidence
There is no direct evidence for public confidence in this particular programme. However, the successful results suggest that the public engaged with the programme and changed their behaviours as a result.
The public demonstrated in the National Party government, which had funded and promoted the programme. The party had won the 1990 general election convincingly, although its victory in the 1993 election was by a much reduced majority.
Clarity of objectives
The key objective was simple and measurable: to reduce and ideally eliminate the incidence of SIDS. It was retained throughout the programme and continued through subsequent interventions, particularly with respect to Maori and Pacific populations, who continue to be at greater risk of SIDS.Strength of evidence
The New Zealand Cot Death Study, a large three-year case control study, was conducted from 1987 to investigate the factors influencing SIDS. The results of this study showed that three key factors increased the risk of SIDS: prone sleeping position, maternal smoking, and lack of breastfeeding. The New Zealand Cot Death Prevention Programme used this evidence to target its initiatives. “For the first time there is solid evidence on which to base intervention to prevent SIDS.” [7]
Evidence was also collected during the programme and any insights gained from this fed back into the ongoing activities of the programme. For example, initial material promoted side or back sleeping. “The effectiveness of the campaign was monitored as it progressed and when it was shown that the original messages had not reduced the SIDS rate in the minority racial group, modifications were recommended. Maori-targeted messages have been produced and a further program for Maori mothers is being developed.” [8]
Not all of the interventions and advertising campaigns used in the prevention programme were piloted or based on existing best practice. Many, however, drew on the 1989 Baby Health Care Kit.
Feasibility
The feasibility was addressed on three main fronts:
- Financial - the costs for the various interventions came out of existing local and national health budgets, with some additional funding from the Hawkes Bay Medical Research Group and the New Zealand Cot Death Association.
- Human resources - the programme utilised existing public health and education practitioners to deliver the programme across the country.
- Legal - the 1990 Act addressed the risk posed by maternal smoking.
Management
The program was coordinated by the Child Adolescent Health Policy Unit of the Department of Health. This involved the preparation of a coordinating plan and strategies, ensuring development and distribution of print resources for parents, liaison with area health boards and other key provider agencies and preparation and distribution of information to key health workers and general practitioners.
Area health boards were asked to appoint one or more coordinators to disseminate the research findings to health workers and to assist with local efforts to promote the three objectives.
A part-time programme coordinator was also appointed to facilitate the sharing of information between the various groups and area health boards.
Individual health practitioners continued to report to their usual managers - the programme was rolled out alongside pre-existing services such as Plunket visits for new mothers and babies.
Measurement
A research project by the New Zealand Cot Death Study Group and the Royal New Zealand Plunket Society monitored the changes in the prevalence of the risk factors identified. “The information is being collected prospectively on every baby by Plunket and public health nurses at initial contact and when the infants are approximately two and four months of age. The data on infants who subsequently die and a random sample of control infants will be extracted from the nursing records and examined by the usual case-control method.” [9]Alignment
The stakeholders and the New Zealand public all agreed that preventing SIDS was desirable. Furthermore, the key stakeholders (DHBs, the Department of Health, and health practitioners) were aligned in their support of the programme. “The plan was shared by all child health agencies who were mutually concerned about the problem of New Zealand's very high SIDS rate.” [10]
The programme coordinator facilitated this alignment by forming a network of relevant groups and holding consultation sessions within the network. “This nationwide network of groups has ensured the acceptance of the results and has ensured that the education of health professionals and the public has delivered one message.” [11]
The political parties were united in supporting the programme, as is evident from a 1991 advertisement. “Two politicians, Mike Moore (Labour) and Winston Peters (National) explain they don't often see eye to eye. But they do see 'nose to nose' on Red Nose Day. Red Nose Appeal, 16 August 1991, supporting research into cot death.” [12]
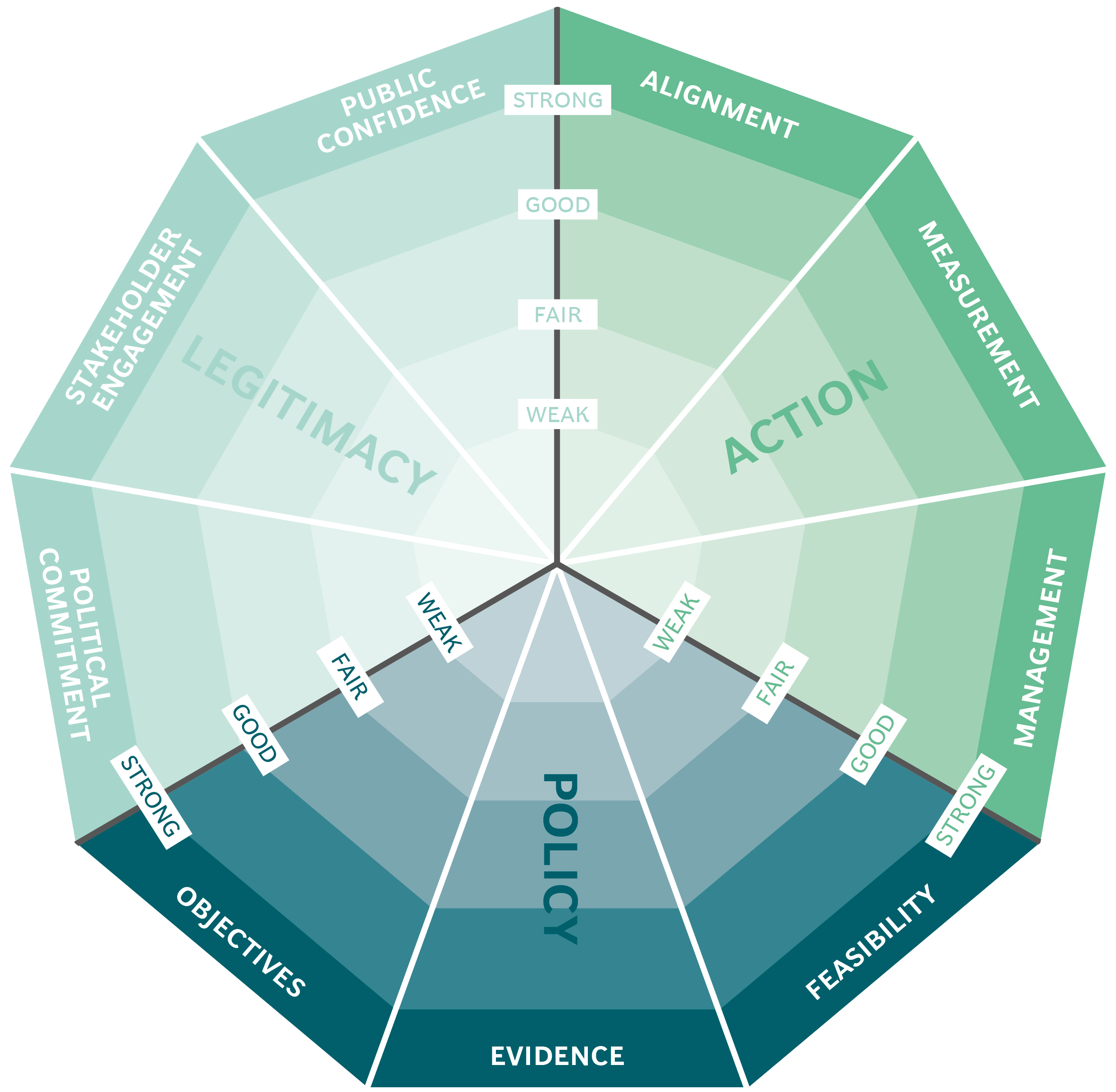
The Public Impact Fundamentals - A framework for successful policy
This case study has been assessed using the Public Impact Fundamentals, a simple framework and practical tool to help you assess your public policies and ensure the three fundamentals - Legitimacy, Policy and Action are embedded in them.
Learn more about the Fundamentals and how you can use them to access your own policies and initiatives.
You may also be interested in...


The Australian Centre for Social Innovation: the Family by Family (FbF) project

Merit-based Girls Scholarship - Kenya

Primary education management in Madagascar

Organ Donations in Iran
