
Legislating to encourage organ donation in Israel
The initiative
The Israeli government designed a new policy that took a pragmatic approach to the problem, “a pioneering approach that gives transplant priority to those willing to contribute to the organ pool.” [3] It was set out in the Organ Transplant Act 2008, which came into effect in January 2010.
“The Act's principal aim is to increase the number of deceased donor organ donations. In order to achieve this, it introduces a priority points system, set out at policy level, intended to motivate individuals to donate their organs.” The three-tiered system is as follows:
- The first priority for transplants is for living donors and the family members of donors.
- Registered donors of three years or more receive second priority.
- Family members of registered donors receive a third tier of priority.
“Another feature of the 2008 Organ Transplant Act [was] full reimbursement to living donors for lost work time, and health and life insurance for five years.” [4] The Act also created a database of registered organ donors.
The challenge
In 2008, Israel provided fewer organ donations than any other Western country. The reasons were to be found in Jewish law, which proscribes desecration of the dead. This has been widely interpreted to mean that Judaism prohibits organ donation.
“Additionally, there were rabbinic issues surrounding the concept of brain death, the state in which organs are typically harvested. [1] As a result, many patients died waiting for organs.” The Israeli parliament, the Knesset, attempted to resolve the issue through new legislation. “In 2008, to assuage the latter group and attract more advocates in the rabbinical community, the Knesset passed the Cerebro-Respiratory Death Act.” [2]
This was not in itself enough to change the situation. The dearth of donated organs in Israel led many Israelis in need of transplants to seek the necessary medical treatment abroad, which in itself carried a high level of risk and cost.
The public impact
A significant impact was felt almost immediately. “Between 2011 and 2013, the number of Israeli living organ donors increased by 67 percent over the preceding three-year period, and the Israeli transplant waiting list contracted in 2013.”
“In 2013 ... there were a record number of transplants in Israel; meanwhile, transplants received by Israeli patients abroad fell to a quarter of their 2007 peak.”
Stakeholder engagement
Although the legislation was drafted after wide ranging consultations with religious leaders, lawyers, NGOs and medical experts, there was resistance from a section of Orthodox Jews. Orthodox Israelis who were opposed to organ harvesting on religious grounds have called the system discriminatory.Political commitment
The government passed two laws in 2008: the Organ Transplant Act and Brain Death Act to encourage legal organ donation in Israel. This indicates the priority that it accorded to the policy, particularly as it was strongly opposed by a significant and vocal community of Orthodox Israelis.Public confidence
A phone survey conducted prior to implementation of the scheme indicated people were willing to donate their organs. 68% of the 695 interviewed said they were willing to donate, although only 16% [5] [6] had already signed a donor card. 85% said they would receive an organ if the need arises. There was still opposition from some Orthodox Israelis.Clarity of objectives
The objectives set for the policy have been clear and the outcome is measurable in terms of change in the number of donors and time taken to exhaust the waiting list in the country:
- Increasing organ donations in Israel.
- Reducing the long waiting list of patients requiring organ transplants.
- Increasing public acceptance of organ donation arising out of brain death.
Strength of evidence
The new system adopted in Israel is based on similar systems in Singapore and the US. “Israel incorporated non-medical factors into organ allocation on a national scale. [7] (It has precedents in Singapore, where opting-out of implied donor consent pushes transplant candidates down the waiting list should they need an organ, and the United States, where living kidney donors have transplant priority status should they likewise need it.)”Feasibility
The reforms required significant legal changes. However, the changes were led by the government who were therefore in a good position to resource the legal changes. The reforms were also contrary to some religious beliefs and therefore were opposed by some Rabbis. However, the government sought support from religious leaders to try and enhance feasibility.Management
Organ donation happens through a national centre, which was created under the 2008 Organ Transplant Act. “The National Transplant Centre, ADI, was established by the Ministry of Health in order to establish a neutral, national body ... to manage and coordinate the organ donation and transplant system in Israel.” [8]Measurement
A national registry is maintained by the National Transplant Centre with details of registered donors and their families, which can be matched to patient needs. “The consent rate from families has already increased, and the number of organs available for patients has increased in parallel. [9] Transplants have so far increased by more than 60 percent over all this year [2012].”Alignment
Provisions in the law ensure that the interests of patients and donors are protected, and there is support from Orthodox rabbis, who are the religious leaders of the Orthodox Israelis. Over 200 Orrthodox rabbis in Israel carry organ donor cards and support organ donation.
The principle of rewards for organ donation has meant that more Israelis are registering themselves as donors. The financial reimbursement provision (see The initiative above) enhanced the participation of people in organ donation and also ensured the wellbeing of the donors.
“Ashkenazi and Sephardi Chief Rabbis of Israel reviewed the medical and halakhic aspects of brain-stem death and concluded that it constitutes the death of the human organism, even while the human organs remain alive. That they ruled organs should be donated.” [10]
The Public Impact Fundamentals - A framework for successful policy
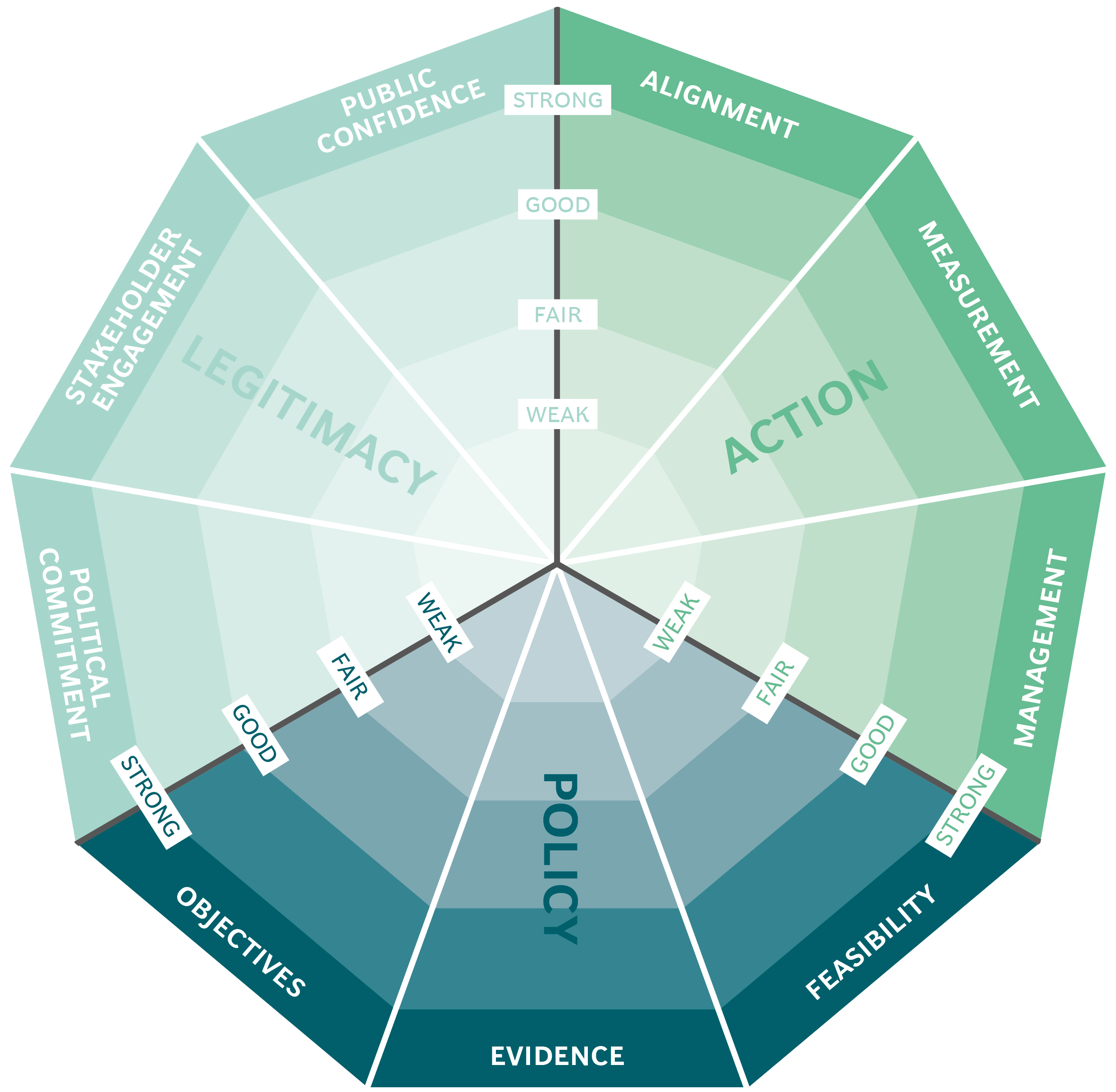
This case study has been assessed using the Public Impact Fundamentals, a simple framework and practical tool to help you assess your public policies and ensure the three fundamentals - Legitimacy, Policy and Action are embedded in them.
Learn more about the Fundamentals and how you can use them to access your own policies and initiatives.
You may also be interested in...


Organ Donations in Iran

GAVI, the vaccine alliance

WHO: delivering insecticide treated nets to control malaria

Mobile technologies for health in Zambia
