
Smoking ban in the United Kingdom
The initiative
In November 2004, the UK Department of Health published the public health white paper, ‘Choosing Health: Making healthy choices easier'.[9][10] The paper was “drawn up after one of the largest public consultations at the time, involving 150,000 people”.[9] It emphasised the pressing need to protect citizens from secondhand smoke and stated that public opinion on the whole favoured legislative intervention. After an additional round of consultations, the ban was effected through the Health Act 2006.[11]
The main provisions are set out in section 2 of the Act: “(1) Premises are smoke-free if they are open to the public... (2) Premises are smoke-free if they are used as a place of work − (a) by more than one person... or (b) where members of the public might attend for the purpose of seeking or receiving goods or services from the person or persons working there.”[11]
Scotland had already banned smoking in public premises and workplaces in March 2006. Wales and Northern Ireland followed in April 2007, and England became the last country in the UK to do so in July 2007.
The challenge
In the 1960s and 1970s, smoking in public places such as buses, trains, cinemas, theatres, public houses and restaurants in the UK was allowed. The same was true of the workplace, where smoking was an accepted part of office life.[2]
Even though evidence had started to show the negative health effects of smoking from the 1950s onwards, the general public and many health professionals largely ignored or dismissed the evidence. The tobacco industry invested in denying and distracting attention from the link between cigarettes and bad health, despite being aware of the health risks posed by smoking.[3]
Throughout the 1970s and 80s, the dangers of smoking − and passive smoking − became more and more apparent to health professionals and the public. Public places and offices in the UK began to impose voluntary and partial smoking bans through the 1980s and 1990s. For example, there was an increasing number of “No Smoking” carriages in trains, the London Underground banned smoking in 1987, and smoking in offices often became confined to one or two rooms before being banned completely.[4][5]
In 2002, a report by the International Agency for Research on Cancer, part of the World Health Organization (WHO), quantified the risks of passive smoking. It concluded that environmental (secondhand) tobacco smoke causes lung cancer among non-smokers.[6] Other reports confirmed these findings: passive smoking was clearly harmful.[7] In 2003, the UK government's chief medical officer, Dr Liam Donaldson, launched his annual report, stating that “voluntary agreements were not reducing the health risks from passive smoking quickly enough”.[5]
In 2005, researchers found that passive smoking “increases the risk of coronary heart disease by approximately 30 percent. This effect is larger than one would expect on the basis of the risks associated with active smoking and the relative doses of tobacco smoke delivered to smokers and non-smokers.”[8] It became evident that partial and voluntary bans were inadequate to protect people from the effects of passive smoking.
The public impact
In the first 18 months after the implementation of the ban, 98.2 percent of premises inspected were found to be compliant.[12] There was a fall in respiratory illness reported by bar workers immediately after the ban. Research also showed that hospital admissions for heart attacks fell by 2.4 percent immediately following the change in the law, which is the equivalent of 1,200 fewer heart attacks per year.[12]
The number of smokers in the UK has also decreased, with less than 15 percent of people smoking in 2019, compared to 22 percent in 2006.[13][14]. Whether this is due to the smoking ban is debatable; however, it is likely that the ban has contributed to the decline in the number of smokers.[15]
A YouGov survey from 2017 also indicated growing support for the smoking ban, with 83 percent supporting the ban as against 78 percent in 2007. It is thought that this shift was mostly due to more smokers supporting the ban.[16][17]
It is harder to separate the longer-term effects of the smoking ban in England. According to the BBC, assessing the full impact of the smoking ban on health will take time, as decreasing rates of lung cancer will only show themselves in the coming decades.[12]
The number of pubs in the UK has fallen since the ban, with almost 7,000 pubs (out of an existing 56,000) closing between 2007 and 2015.[12] While some attribute this to the smoking ban, it is difficult to determine whether the decreasing number of pubs may have been caused by the ban, the onset of the financial crisis of 2007, changing attitudes towards drinking, or other factors. It is recognised, however, that the smoking ban has changed the pub landscape; pubs have become more family-friendly and more like restaurants, and many of the traditional pubs have had to change their business models to survive.[18]
Today, the UK is at the forefront of tobacco policy, leading the European league table for tobacco control.[1] “When the legislation was introduced, England was following the herd... Over the past decade there has been a flurry of new legislation − and the UK has often been at the forefront.”[12] Since 2007, England has increased the age at which tobacco products can be purchased, introduced picture warnings on packaging, banned the sale of cigarettes through vending machines and rolled out standardised packaging for tobacco products. The smoking ban seems to have not only improved public health but also inaugurated an era of comprehensive tobacco policy.
Written by Margot Gagliani
Stakeholder engagement
The main stakeholders of the smoking ban were medical professionals, local councils, the owners of licensed premises and others who were obliged to comply with the 2006 Act, the police, and the general public.
As is customary with significant legislation in England, there was a comprehensive consultation process with all stakeholders when drafting and reviewing the white paper. The policy was designed with their input in mind, particularly that of the medical profession, through bodies such as the British Medical Association, not-for-profits such as the King's Fund, and the National Health Service trusts responsible for hospitals and clinics.[10]
The main resistance to the change came from pro-smoking pressure groups and the owners of licensed premises such as pubs. The owners and employees of “wet pubs” (those that would get the majority of revenues from drinking customers) were especially worried about the effect the ban would have on their clientele and revenue.[18]
However, the UK's largest pub chain, JD Wetherspoon, said that “the smoking ban would be good for business”.[9] By May 2006, more than a year before the official ban, the pub chain had already banned smoking in all its premises. This led to a recognition by many other pub owners that the legislation had public support and that it was part of an inevitable progression.
Political commitment
The government was committed to the legislation, which was seen as having major public benefits. The then health secretary, Patricia Hewitt, was a vocal proponent, as was Dr Liam Donaldson.[5]
In November 2004, the government published the white paper on public health, detailing its intention to introduce the provisions in smoke-free premises. The Health Bill was drafted in light of the consultation process following the white paper's publication. It received its first reading in parliament on 27 October 2005.
On 14 February 2006, after the third reading of the Health Bill, MPs voted by 364 votes to 21 in favour, and it was therefore approved to pass into statute.[19] This large majority in favour of the bill indicates that there was strong commitment to the smoking ban and that this was not a party political issue.
Public confidence
As the Institute for Government said, “the final policy was the culmination of a popular consensus that government was right to intervene in matters of public health... By 2006, public opinion appeared to strongly favour a comprehensive ban.”[5]
Public support in favour of smoke-free premises had been growing in the years leading up to the smoking ban. In 2004, a MORI opinion poll indicated that there was a slight majority of 54 percent in favour of a smoking ban.[20] In 2007, at the time when the 2006 Act came into effect, 78 percent of the public were in favour of the legislation, which would grow to 83 percent by 2017.[17]
Clarity of objectives
As the white paper had set out, the government's broad objective was to improve public health by reducing the negative effects of secondhand smoke. It was made clear that this would be achieved through a ban, as the existing voluntary regulations were seen as insufficient to protect people from the adverse health effects of passive smoking.[9][5]
It was also thought that this would have a positive effect on smokers by encouraging them to give up or reduce smoking.
Strength of evidence
The Choosing Health white paper was based on extensive evidence favouring a ban.[10] The evidence suggested both that tobacco smoke substantially harms passive smokers and that a ban could be an appropriate tool to address this issue.
A large body of evidence suggested that secondhand smoke increases the risk of cancer, coronary disease and other illnesses (see The Challenge above).[6][7][8] The WHO also recognised the increased health risks of passive smoking to those working in licensed premises [23].
A similar ban had been enforced in New York in 2003, under the New York City Smoke-Free Air Act of 2002. In March 2004, Ireland became the first European country to institute an outright ban on smoking in the workplace. This provided evidence that such bans were enforceable. The members of the House of Commons Health Select Committee also visited Ireland in order to be able to see the ban in practice.[5]
There was evidence from the WHO that legal restrictions − when carefully planned − would be effective in reducing the consumption of tobacco.[22] Additionally, a 2003 review of 97 studies from around the world had shown that a smoking ban would not necessarily harm the hospitality and pub industry by reducing sales or employment.[21]
Feasibility
The fact that there had been a gradual movement towards banning smoking in workplaces and enclosed public spaces helped the feasibility of implementing a complete ban. It was becoming increasingly socially unacceptable to smoke in enclosed spaces, the medical evidence was considered to be very credible, public opinion was behind the ban, and the consultation process on the 2004 white paper indicated that the vast majority of public bodies approved of the smoke-free provisions.[5] This facilitated the implementation of the ban, as it became increasingly easier to enforce the regulation.
The progress towards the smoking ban had been gradual but relentless, including anti-smoking legislation such as the Tobacco Advertising and Promotion Act 2002; this indicated that the 2006 Act would be successful in terms of both enforcement and compliance.
Additionally, licensed premises in the UK were already highly regulated.[24] Measuring compliance with the ban was therefore feasible under the normal inspections regime, and would not require a large additional investment.
Management
The 2006 Act made clear provisions for enforcement of the act in relevant premises, and imposed penalties on those contravening or failing to enforce the ban.[11] Owners or managers of any relevant premises had to display “No smoking” signs and take reasonable steps to ensure awareness of the ban and compliance with it.
Local councils were in charge of enforcing the law, and extra officers were taken on to ensure compliance.[25]
Measurement
There were several parameters that were measured over time to monitor the success of the initiative, such as compliance rates, the health of those working in licensed premises, and hospital admissions for particular smoking-related infections. “A study of bar workers in England showed that their exposure reduced on average between 73 percent and 91 percent and measures of their respiratory health significantly improved after the introduction of the legislation... In England, the legislation resulted in a statistically significant reduction (-2.4 percent) in the number of hospital admissions for myocardial infarction (MI). This amounted to 1,200 emergency admissions for MI in the year following the introduction of smoke-free legislation.”[26]Alignment
There was a clear alignment of interests between the government, citizens and medical professionals in introducing a ban. There was significant cooperation between the government and the parties who were consulted on the white paper to ensure that the Health Bill reflected expert and general opinion. There was also cooperation between the various political parties, as reflected in the very large majority when the bill was voted on in parliament.
Initially, there was opposition to the ban from owners of licensed premises as well as pro-smoking lobbying groups. However, over time, the 2006 Act's effects on many of such premises proved less severe than anticipated, and smoking has become increasingly socially unacceptable; accordingly, the level of opposition declined.[18] At the same time, the tobacco industry has had to concede the negative health effects of smoking and secondhand smoke.[27]
Bibliography
[1]. Global Public Policy: does the new venue for transnational tobacco control challenge the old way of doing things? H. Mamudu, P. Cairney and D. Studlar, 15 January 2015, Public Administration, 93, 4, 856-873, https://onlinelibrary.wiley.com/doi/abs/10.1111/padm.12143
[2] Smoking and health 50 years on from landmark report, Dominic Hughes, 6 March 2012, BBC, https://www.bbc.co.uk/news/health-17264442
[3] The history of the discovery of the cigarette-lung cancer link: evidentiary traditions, corporate denial, global toll, Robert Proctor, 2011 (corrected 1 January 2013), The BMJ, https://tobaccocontrol.bmj.com/content/21/2/87
[4] Smoking in Public Places Investigate Committee, Greater London Authority, March 2002, https://www.london.gov.uk/sites/default/files/gla_migrate_files_destination/archives/assembly-reports-health-smoking_report.pdf
[5] The Ban on Smoking in Public Places (2007), 2011, Institute for Government, https://www.instituteforgovernment.org.uk/sites/default/files/smoking_in_public_places.pdf
[6] Passive smoking, Allan Hackshaw, 28 August 2003, The BMJ, https://dx.doi.org/10.1136 percent2Fbmj.327.7413.501-b
[7] BMA steps up call for ban on smoking in public places, Anne Guland, 2002, The BMJ, https://doi.org/10.1136/bmj.325.7372.1058/a
[8] Cardiovascular effects of secondhand smoke: nearly as large as smoking, Joaquin Barnoya and Stanton A. Glantz, 24 May 2005, Circulation, https://doi.org/10.1161/CIRCULATIONAHA.104.492215
[9] Smoking ban proposed for England, 16 November 2004, BBC News, http://news.bbc.co.uk/1/hi/health/4014597.stm
[10] Choosing Health: Making healthy choices easier (alternative title − Public Health White Paper), Department of Health,16 November 2004, The National Archives, https://webarchive.nationalarchives.gov.uk/+/http://www.dh.gov.uk/en/Publicationsandstatistics/Publications/PublicationsPolicyAndGuidance/DH_4094550
[11] Health Act 2006, legislation.gov.uk, https://www.legislation.gov.uk/ukpga/2006/28/contents
[12] Pub smoking ban: 10 charts that show the impact, Nick Triggle, 1 July 2017, BBC News, https://www.bbc.co.uk/news/health-40444460
[13] Turning the tide on tobacco: Smoking in England hits a new low, Duncan Selbie, 3 July 2018, Public Health Matters, https://publichealthmatters.blog.gov.uk/2018/07/03/turning-the-tide-on-tobacco-smoking-in-england-hits-a-new-low/
[14] Smoking statistics: who smokes and how much, February 2016, Ash (Action on Smoking and Health), http://ash.org.uk/wp-content/uploads/2016/06/Smoking-Statistics-Who-Smokes-and-How-Much.pdf
[15] Smokers back extension of ban to play areas and cars carrying children, Jamie Doward, 27 June 2010, The Guardian, https://www.theguardian.com/lifeandstyle/2010/jun/27/smoking-ban-cars-with-children
[16] England a decade after the smoking ban - heading for a smokefree future, 1 July 2017, Ash (Action on Smoking on Health), http://ash.org.uk/media-and-news/press-releases-media-and-news/england-a-decade-after-the-smoking-ban-heading-for-a-smokefree-future/
[17] Smoking ban: Number of UK smokers falls by nearly two million in 10 years, Katie Forster, 1 July 2017, The Independent, https://www.independent.co.uk/news/health/smoking-ban-uk-smokers-numbers-fall-two-million-19-cigarettes-tobacco-drop-10-years-a7817236.html
[18] A breath of fresh air: how the smoking ban has changed the pub trade, Claire Churchard and Georgina Townshend, 18 June 2017, The Morning Advertiser, https://www.morningadvertiser.co.uk/Article/2017/06/19/How-the-pub-trade-has-changed-since-the-2007-smoking-ban
[19] The St Valentine's Day Manifesto Massacre: The Smoking Votes, Philip Cowley and Mark Stuart, 14 February 2006, Revolts, http://www.revolts.co.uk/Smoking percent20Vote percent2014 percent20Feb percent2006.pdf
[20] Select Committee on Health: First Report, Annex 2: Public opinion, June 2005, UK Parliament, https://publications.parliament.uk/pa/cm200506/cmselect/cmhealth/485/48515.htm
[21] Review of the quality of studies on the economic effects of smoke-free policies on the hospitality industry, M Scollo, A Lal, A Hyland and S A Glantz, 1 March 2003, Tobacco Control, https://tobaccocontrol.bmj.com/content/tobaccocontrol/12/1/13.full.pdf
[22] Which are the most effective and cost-effective interventions for tobacco control? August 2003, World Health Organization, http://www.euro.who.int/__data/assets/pdf_file/0004/74722/E82993.pdf
[23] Smoking in Public Places: First Report of Session 2005-06, House of Commons Health Committee, 15 December 2005, UK Parliament, https://publications.parliament.uk/pa/cm200506/cmselect/cmhealth/485/485.pdf
[24] The Pubs Code etc. Regulations 2016, 2016, legislation.gov.uk, https://www.legislation.gov.uk/ukdsi/2016/9780111147481/contents
[25] Advice on smoking at work, 2019, Health and Safety Executive, http://www.hse.gov.uk/contact/faqs/smoking.htm
[26] Smoking ban, 2019, politics.co.uk, https://www.politics.co.uk/reference/smoking-ban
[27] Tobacco Industry, 2019, Ash (Action on Smoking and Health), http://ash.org.uk/category/information-and-resources/tobacco-industry-information-and-resources/
#GPS
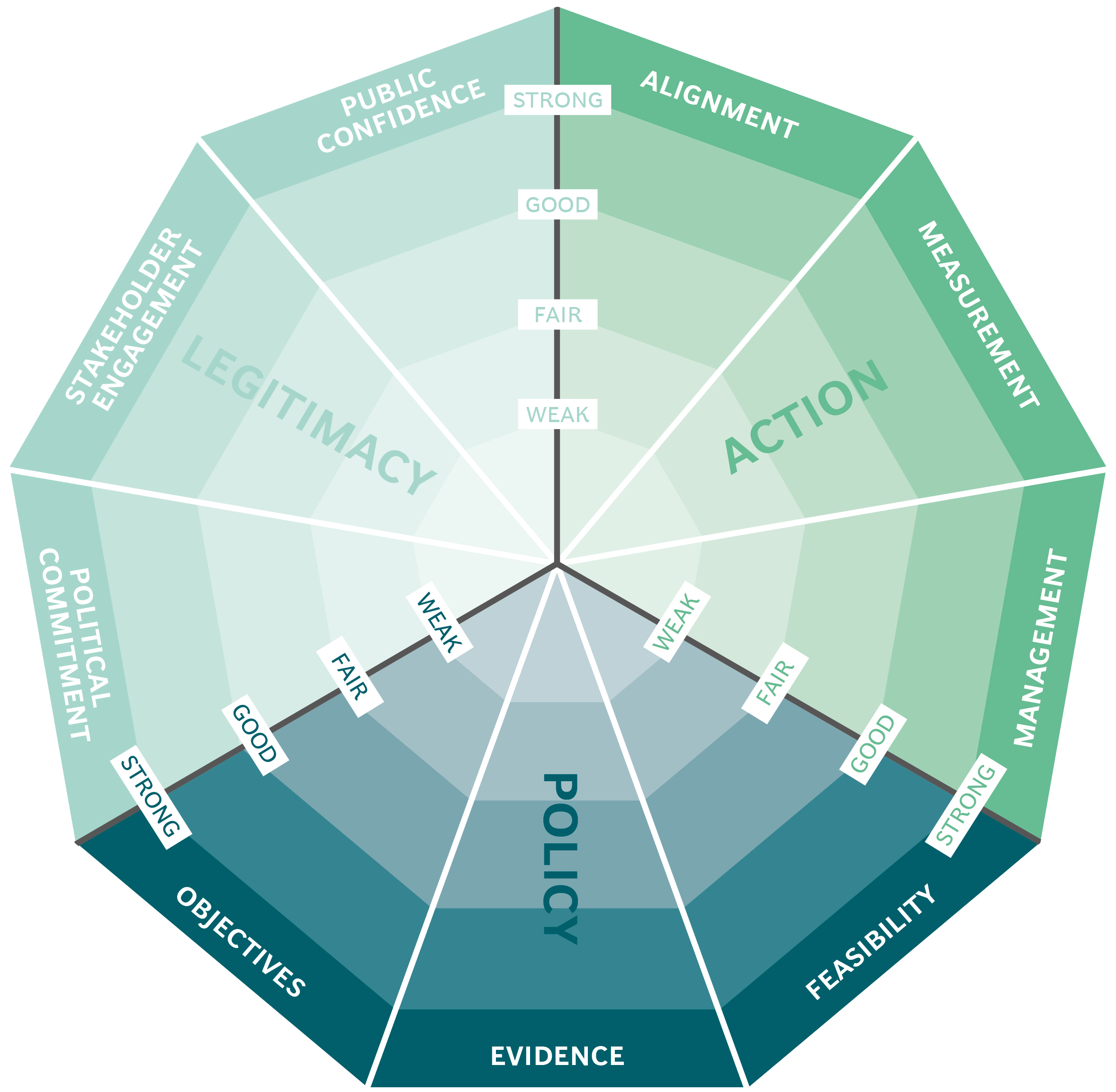
The Public Impact Fundamentals - A framework for successful policy
This case study has been assessed using the Public Impact Fundamentals, a simple framework and practical tool to help you assess your public policies and ensure the three fundamentals - Legitimacy, Policy and Action are embedded in them.
Learn more about the Fundamentals and how you can use them to access your own policies and initiatives.
You may also be interested in...


The Australian Centre for Social Innovation: the Family by Family (FbF) project

Merit-based Girls Scholarship - Kenya

Primary education management in Madagascar

Organ Donations in Iran
