
Piri Pono – a peer-led acute residential service in New Zealand
Feedback from service users and families who attended the North Shore Hospital in Auckland, New Zealand in 2010 showed that acute inpatient care for people with mental health conditions could be traumatic. Instead, they advocated alternative, community care services close to home. Meanwhile, hospitals were looking to cut the number of costly inpatient hospital beds. As a result, it was agreed to open up Piri Pono, a short-term, peer-led, acute residential service with five beds, in Rodney, Auckland. The service was based on similar peer-based respite services but was the first peer-led acute mental health service in the Waitematā district that also offered therapeutic interventions, and one of only three peer-led services in the whole country.
Initially, some clinicians were doubtful that an acute service could be peer-led, but the subsequent success of the centre has started to change those views. It even led to the centre being featured in He Ara Oranga - Report of the Government Inquiry into Mental Health and Addiction 2018 as a positive example of peer-led, community-based alternatives to hospitalisation. In the first 18 months, 80 percent of guests at Piri Pono agreed that the staff and service were inspiring and encouraging and 84 percent reported a reduction in distress following their stay at Piri Pono.
The initiative
In 2013, the Waitematā DHB, together with Connect Support and Recovery Inc (now part of Ember - Korowai Takitini) and Rodney Adult Mental Health Services, set up a peer-led acute residential service called Piri Pono to act as an alternative to acute inpatient care.[2] The name Piri Pono means “loyal” in Māori.[2] Darryl Bishop, Group CEO at Ember - Korowai Takitini summarised the reasoning behind the formation of Piri Pono as; “The desire for more community beds away from hospital, and the desire for more peer services, kind of crunched together to create Piri Pono.”[3]
Piri Pono is located in Silverdale and serves the North Shore and Rodney communities in Auckland. It provides a community-based alternative to hospital admission for people experiencing acute mental health conditions, through a maximum ten-day stay in a homelike environment. Employing staff with lived experience of mental health conditions is a core element of Piri Pono's therapeutic approach, and the service offers therapy as well as acting as a respite home. Although there are other peer-led organisations in New Zealand, such as Centre 401 in Hamilton, they are slightly different from Piri Pono as they are more respite-oriented.[3][4] Darryl Bishop explains how Piri Pono is different from a respite home; “Because [Piri Pono] is supposed to be, well, it is, a therapeutic unit. It's not just a place of holding. It's a place where people receive peer support work. So they are being treated for the time they're there, in the intentional peer support model. It's a very busy therapeutic space. It's not based on just being there and somebody with lived experience just taking care of you.”[3]
The challenge
In 2010, there was a growing need to develop community-based mental health options in New Zealand in order to reduce the cost of mental health services and provide a more effective means of treatment to service users. Inpatient care at hospitals is expensive, making up about 30 percent of the total cost of services.[1] A large proportion of the cost of acute inpatient care is generated by long or repeat admissions for a small number of service users. Backed by evidence suggesting that some of these admissions could be avoided with better community care, the New Zealand government was in favour of promoting improved community services in order to reduce overall costs.[1]
Feedback from service users and their families was collected in relation to a rebuild project at the North Shore Hospital in Auckland in 2010. It demonstrated that some people found the experience of admission to inpatient units traumatic, and a common theme was to favour a more community care-based alternative over the traditional institutional care.[2] “It should be acknowledged that inpatient admissions can be traumatic; they increase both societal and self-stigma; and have been criticised by service users as acting as holding places, rather than for therapeutic benefit.”[2]
The leadership of the Waitematā District Health Board (DHB) therefore decided against replacing the sub-acute beds with hospital beds and opted to look at alternative, community-based options instead. Although 90 percent of service users accessed community services, there were only two peer-led services available in the whole of New Zealand, the Centre 401 in Hamilton and Tupu Ake in Papatoetoe.
The public impact
Piri Pono uses a range of methods to regularly evaluate the impact of its service on the mental wellbeing of its guests and to understand the experience of its staff. Results from Piri Pono's first 18 months showed positive results across all 4 evaluation methods. Specifically, guests' feedback indicated that 80 percent of guests strongly agreed that the staff and service were inspiring and encouraging.
The major themes emerging from the guests' post admission reflective survey included the importance of others having experienced mental illness or distress themselves, and the value of connecting with others, being understood, and not being judged. In all, 84 percent of the 62 guests who completed the Kessler 10 Psychological Distress Scale experienced a reduction in self-reported measures of distress. In addition, 80 percent of guests agreed that the staff and service were inspiring and encouraging, and 84 percent reported a reduction in distress following their stay at Piri Pono.[2] “Particular strengths of Piri Pono appear to be in its staffing, which was described positively by guests, who appreciated that peer support staff had ‘been there'.”[2]
The choice of registered nurses with lived experience is especially noteworthy.[2] One guest commented: “I am inspired by this service on a personal and professional level, it's a great place. No other service I have had contact with has been so valuing and respectful of me and understands so much of my struggle. I don't know how this works on paper, the idea of peer support programmes in crisis look like a major risk/hazard, but they have pulled it off here and it's truly remarkable. We need more of them.”[2]
The staff themselves also spoke positively about Piri Pono. “By the time it comes to exiting or planning their exit, they've got a least two or three different goals, be they just small or big... but the general kind of thing that you see is people really brightening up, body language changes; they're speaking and making eye contact.”[2]
The success of the centre was highlighted as a positive example in He Ara Oranga - Report of the Government Inquiry into Mental Health and Addiction, published in 2018. “Several relatively new community-based acute alternatives to hospitalisation are showing great results for people who would otherwise be admitted to inpatient acute units. One of these is Piri Pono... Evaluations of Piri Pono have been positive, and tāngata whaiora and their families and whānau view it favourably.”[5]
Stakeholder engagement
There was clear stakeholder commitment from the three main partners - Waitematā DHB, Connect Support and Recovery (now Ember - Korowai Takitini) and Rodney Adult Mental Health Services. The successful engagement was due to clear communication, shared decision-making, and the fact that some stakeholders had lived experience of mental health issues and already understood the benefits of peer-led mental health services.[3] The funders valued the cost-effective service provided by Piri Pono, and their support for a peer-led service was enhanced by the presence of a board member with lived experience.[3]
The Rodney Adult Community Mental Health Service, which covers the semirural district where Piri Pono is located, has benefited from being able to offer local mental health treatment options for the population closer than the North Shore hospital in Auckland. Connect Support and Recovery were, in turn, very knowledgeable about peer-led acute services and played a key role in ensuring that all stakeholders shared the same vision.[3] “The engagement was very good. The steering group that exists there was still made up of representatives from us, as a service provider, from the DHB, as the funder, and also from the local mental health service provider. So that remained and remains really strong.”[3]
Political commitment
There was a good level of political commitment for the initiative, thanks to cross-party support and a clear national policy emphasis on backing peer-based services, as set out in the Mental Health Commission 2012 Blueprint II report.[6] “We need to ensure that there is a coherent spectrum of evidence-based self care options available including mental health and addiction health literacy, e-therapies, and whānau and peer support.”[6] The national and local policy was to have more beds in the mental health system to cater for a growing population, but not more hospital beds.[3]
However, even though the evidence of political commitment is available in terms of rhetoric and written policy, the number of peer support workers has not increased since 2012. “I think everybody talks about peer services being something that is a growing part of mental health services in New Zealand. But the number of FTEs [full-time equivalents] up here to support workers is the same now as it pretty much was five years ago.”[3]
Public confidence
There is not enough information to assess the level of public confidence for Piri Pono.Clarity of objectives
Piri Pono's objectives are clearly stated in the August 2016 document, Piri Pono: Evaluation of the Peer-Led Acute Alternative Service, namely to:
- Rapidly enable service users/tāngata whaiora to reduce stress levels, enhance wellness, and strengthen their ability to maintain their safety within the community
- Provide a service and setting that is valued by service users/tāngata whaiora who access it, and that is experienced as welcoming, safe, comfortable and supportive
- Minimise the need for hospitalisation by actively supporting service user/tāngata whaiora in the community
- Provide a homelike, comfortable environment for the provision of recovery-focused support and treatment
- Work collaboratively with the users/tāngata whaiora, Waitematā DHB Clinical Services, and any other mental health services to ensure quality care is provided to service users
- Provide a welcoming environment, which is valued by visiting family/whanau.[2]
Most of the objectives are measurable and continuously monitored, using evaluation tools such as different forms of surveys and focus groups, occupancy rates and referrals to capture the performance of Piri Pono against its objectives. One set of results from the first 18 months has been reported, and another set of results from the following 18 months has just been completed.
Strength of evidence
There was a substantial evidence base for the project, as findings from research, feedback studies, and previous peer-led mental health service projects were used to inform its planning. Specifically, Connect Support and Recovery looked at other, existing models to inform the development of their own model.[3] “They looked at Wellington, they looked at a couple of models overseas. And they developed basically a bespoke solution for our community, based on what the best of what they had seen overseas.”[3]Feasibility
Feasibility for the Piri Pono project was good, thanks to the strong and continuous support from its funders and the board.[3] In addition, the fact that the concept of Piri Pono as a peer-based, acute service in a community setting echoed the national mental health policy of reducing the number of hospital beds in favour of community-based alternatives also supported the project's feasibility.
Feasibility relating to skilled and trained staff was also good, as all the peer support workers received training in Intentional Peer Support (IPS). “So we treat IPS, the intentional peer support model incredibly seriously. Not just in the training, but also in terms of refreshers and the supervision structures that go in place. Because often the misunderstanding of peer support is that it's just support from people with lived experience, but... intentional peer support is as technical and as a detailed model as CBT or DBT or MST or any of the T's that you like.”[3] (The reference is to Cognitive Behavioural Therapy, Dialectical Behaviour Therapy, and Multisystemic Therapy.)
However, financial feasibility was weaker, due to the chosen funding model. Initially, there had been an intention to establish further units like Piri Pono, which could share staff and thereby reduce the running costs. However, due to a lack of government funding, this has not yet happened. The project is on a five-year funding contract, which has been renewed in 2019 for another five years. As Piri Pono offers therapeutic interventions, there are higher demands on providing qualified and clinical staff than in a respite home. “So we could just run it like a sort of peer respite service and not have as many staff there. But we don't want to do that. We always wanted to run an acute alternative. So, really, five beds don't work... If we were doing it again, I think we'd be a bit stronger about insisting it was at least six beds, so that it could break even.”[3]
Management
Management of the Piri Pono project was strong, both at the higher and lower levels of the management structure. The Waitematā DHB, Connect Support and Recovery, and Rodney Adult Community Mental Health Service had clear roles and responsibilities. Ember - Korowai Takitini, which was established through the merger of Connect Supporting Recovery and the Framework Trust, now manages Piri Pono and works collaboratively with Waitematā District Health Board funders, managers, and clinical teams. The Rodney Adult Community Mental Health Service acts as the single point of entry and manages the admission process, as Piri Pono is located in its catchment area.[3] Clinical responsibility for service users lies with the Waitematā DHB clinical teams of Rodney and the North Shore in Auckland. “Clinicians are expected to visit daily with regular Consultant Psychiatrist assessments and treatment throughout an individual's stay. A registered nurse (RN) employed by Connect Supporting Recovery is available on site 9 am to 9 pm.”[2]
During the implementation stage, a steering group was also established to oversee the project's developments and to focus on the implementation of the service objectives. “The group included representation from the Rodney Community Mental Health team; consultant psychiatrist, Red Beach Consumer Advisor, clinical specialist, funders and managers and family and cultural advisor, as well as senior Connect Supporting Recovery staff.”[2]
To help ensure that Piri Pono's peer support aspect was understood by all those who managed it, lived experience was represented throughout the different management structures, such as staff on the ground, the team managers and the board.[3] Further, the IPS model of working was integral to managing the service, and in-house IPS training and experienced IPS supervisors were used. “It's all about keeping people in the [IPS] model. So, the model's based on mutuality. So if somebody's stuck and they're working with somebody, then we're constantly reminding them what the model says and bringing them back to the model.”[3]
Measurement
Measurement of the impacts of Piri Pono was strong, because the management group set up a comprehensive measurement approach and, in response to the results, actively modified its service in order to improve it.[2] This internal evaluation approach included developing a measurement framework, conducting a study within the public sector six years into the implementation process, and constantly collecting performance data.[2]
The first 18 months of the Piri Pono's operation was evaluated using a specially developed assessment framework, and “data was collected via 4 methods:
- “Satisfaction Survey: completed by guests on the day they exit the service
- “Kessler 10/K10: self-administered distress rating scale provided to guests to complete upon entry and exit of Piri Pono
- ”Reflective survey: an open-ended evaluation survey of the service sent out 4-6 weeks after guests exit
- “Staff Focus Groups: Both Piri Pono and staff of Waitematā DHB were included.”[2]
The conclusion was that: “the active process of gathering evaluation data throughout the first 18 months improved Piri Pono's ability to modify and develop the service; one clear example of this is in the area of activities, which has grown with feedback from service users.”[2]
Alignment
Alignment between the different parties was generally good, because people with lived experience who understood the peer support model were represented in the different management structures.[3]
The importance of understanding the peer support model becomes apparent when looking at the areas where alignment was less successful. Referrals from the North Shore Hospital are sometimes ineligible for Piri Pono's service according to its admission criteria, but are nevertheless directed towards Piri Pono for respite care, due to a lack of beds at the psychiatric unit. This has been a source of tension, because clinicians at the hospital sometimes did not see the difference between Piri Pono and respite services. Piri Pono has resolved this by using Rodney Mental Health Services as a gatekeeper for referrals, but also by allowing occasional non-eligible referrals to stay at Piri Pono.[3]
In addition, there has been scepticism from some medical professionals about the credibility of peer-led acute units. With time, though, Piri Pono has been able to demonstrate their success and ultimately change many of those views. “We've certainly seen that, we had people who were reluctant to refer there who now refer there. So I think we've won many of them over, over time.”[3]
Bibliography
https://www.health.govt.nz/system/files/documents/publications/odmh-arpt10-20mar12.pdf
- Piri Pono: Evaluation of the Peer Led Acute Alternative Service, August 2016, Connect Supporting Recovery and Waitematā District Health Board
- Interview with Darryl Bishop, Group CEO at Ember - Korowai Takitini, 24 August 2019
https://www.mentalhealth.inquiry.govt.nz/assets/Summary-reports/He-Ara-Oranga.pdf
https://www.hdc.org.nz/media/1075/blueprint-ii-how-things-need-to-be.pdf
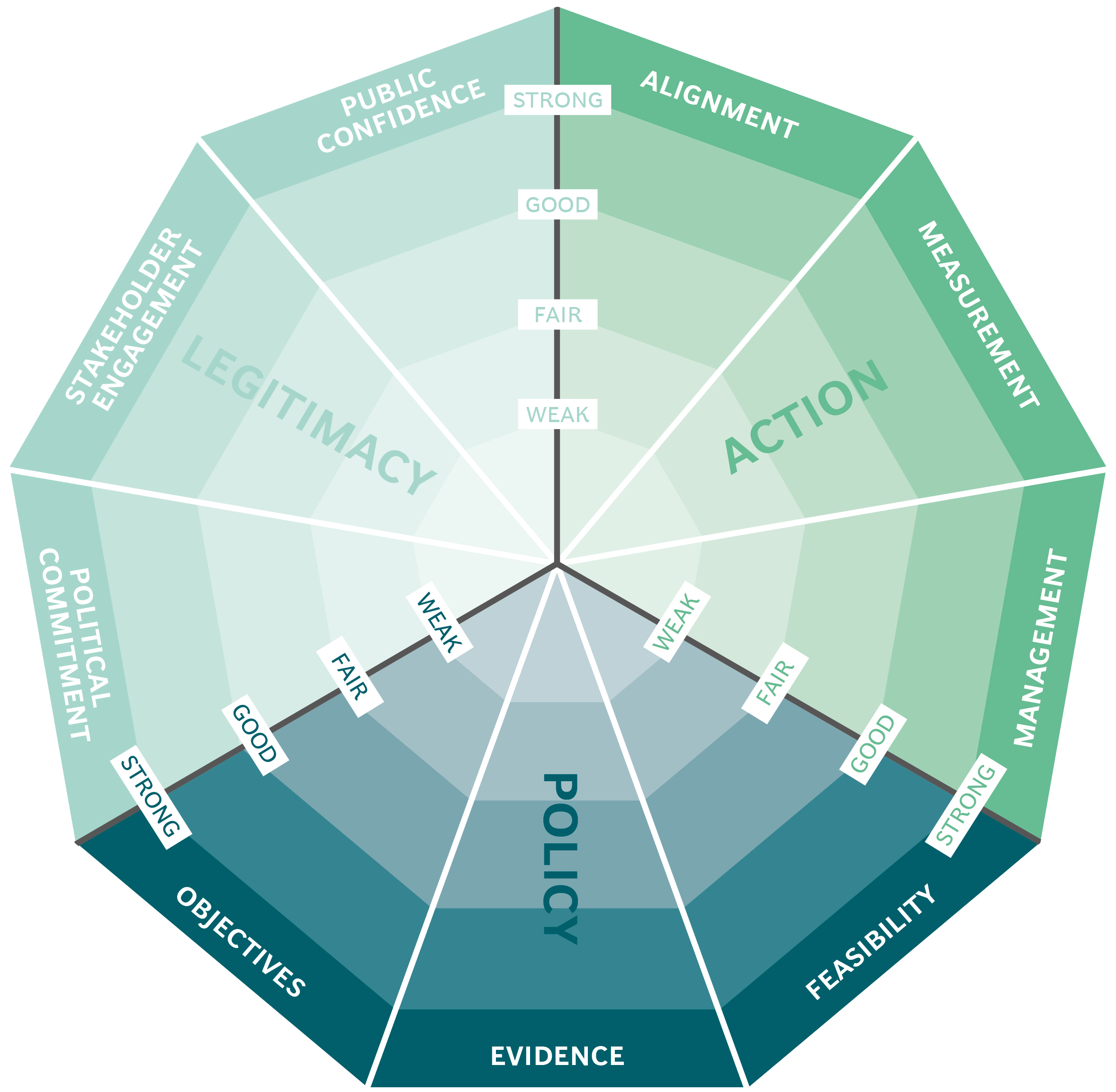
The Public Impact Fundamentals - A framework for successful policy
This case study has been assessed using the Public Impact Fundamentals, a simple framework and practical tool to help you assess your public policies and ensure the three fundamentals - Legitimacy, Policy and Action are embedded in them.
Learn more about the Fundamentals and how you can use them to access your own policies and initiatives.
You may also be interested in...


Organ Donations in Iran

Legislating to encourage organ donation in Israel

GAVI, the vaccine alliance

WHO: delivering insecticide treated nets to control malaria
