
The WHO’s Ebola Virus Disease Outbreak Response Plan
The initiative
The WHO convened a special ministerial meeting about the outbreak of EVD. The meeting was held on 2-3 July 2014 in Accra, Ghana. “[It] brought together ministers of health and senior health officials from 11 African countries ... as well as response partners, Ebola survivors, representatives of airlines and mining companies, and the donor communities." [3] The outcome of this meeting was the WHO's Ebola Virus Disease Outbreak Response Plan in West Africa (the Plan).
Its overriding objectives were to:
- “Stop transmission of EVD in the affected countries through scaling up effective, evidence-based outbreak control measures.
- “Prevent the spread of EVD to the neighbouring at-risk countries through strengthening epidemic preparedness and response measures."
The challenge
Ebola was first seen in the West African nation of Guinea: "a ‘mysterious' disease began silently spreading in a small village in Guinea on 26 December 2013 but was not identified as Ebola until 21 March 2014." [1] On that day Guinea's Ministry of Health notified the World Health Organization (WHO) of a rapidly evolving outbreak of Ebola. On 30 March 2014, Liberia reported its first cases of Ebola, followed by Sierra Leone on 25 May.
In all, a great number of people died from Ebola - known as Ebola virus disease (EVD). While small outbreaks occurred in other African countries, the outbreak in West Africa was by far the largest, longest and most complex. [1] As of 13 April 2016, there [had] been almost 28,652 reported, confirmed, probable and suspected cases of EVD, with 1,325 reported deaths. The majority of deaths were in Guinea (2,544), Liberia (4,810) and Sierra Leone (3,956) with a few in Mali (6), Nigeria (8) and the US (1). [2]
EVD also had a significant effect on the economy and education. “National economies became isolated with stalemates in key sectors. Many people lost employment, and agricultural fields [were] abandoned. The education of an estimated 5 million children and youth [was] set back. [3] Additional expenditure to contain the EVD crisis amidst drastic shortfalls in domestic revenue increased national deficits."
The public impact
“The national and international responses resulted in a number of public health improvements within the three West African nations of Guinea, Liberia and Sierra Leone, including safer burial practices, earlier case detections, more health workers and treatment facilities, public awareness campaigns and stepped-up contact tracing". [4]
The WHO declared the Ebola outbreak to be over on the 9th of June 2016 when Liberia was the last country to be declared Ebola-free (for the third time). It is believed that all known chains of transmission have now been stopped in the West Africa.
Stakeholder engagement
Key stakeholders were in attendance at the special ministerial meeting in July 2014. They shared a common interest: eradicating Ebola. The meeting “brought together ministers of health and senior health officials from 11 African countries ... as well as response partners, Ebola survivors, representatives of airlines and mining companies, and the donor communities." [3] However, the WHO was criticised for failing to failing to adequately engage stakeholders early on in the crisis. [5]Political commitment
The leaders of the three African nations demonstrated leadership once the scale of the epidemic was known. However, there was not a concerted effort on part of the national governments to control the situation when Ebola first started to spread. “Initially information was not shared, and warnings were not disseminated widely enough. Countries hesitated to declare an emergency for fear of creating panic and scaring away business.” [6]
Insights from the local authorities, who were familiar with the local situation, were ignored. “Officials in capitals also initially ignored local authorities, who were sometimes more familiar with traditional customs and accepted by their communities (with the exception of Guinée Forestière, where local authorities were no more familiar with local customs or trusted than the national government)." [6]
The wider international response was also no more effective initially than that of the three countries most affected by the epidemic. The World Health Organization was strongly criticised for its delay in developing a response plan to the outbreak. However, once the Response Plan was developed, the WHO played a clearer, coordinating leadership role.
Public confidence
Although there were reasonable levels of confidence in the United Nations and the WHO as an institution, the response effort was limited by a lack of trust and dialogue between states, response partners and citizens. “The virus initially spread unchecked [partly] because people were sceptical of what their governments were saying or asking them to do. Lack of trust in government intentions, whether in the form of political opportunism or corruption, was based on experience. In its initial phase, many West Africans thought Ebola was a ploy to generate more aid funding or reinforce the position of ruling elites.” [6]Clarity of objectives
The objectives were clearly defined and maintained throughout the life of the Plan: to stop transmission of EVD in the affected countries and prevent its spread to other countries, particularly neighbouring nations in West Africa. [3]Strength of evidence
The Plan developed by the WHO was based upon the collective experience it had gained in response to similar epidemics, such as SARS, pandemic influenza A(H1N1), and Middle East respiratory syndrome coronavirus (MERS-CoV). [3] The health NGOs had also learned lessons from the various outbreaks of Ebola Haemorrhagic Fever in Africa during the 2000s, especially in the Democratic Republic of the Congo and Uganda.Feasibility
The Response Plan was well costed, requesting US$71,053,413 to implement the Ebola outbreak response plans and priority preparedness activities for the period of 6 months to accelerate the response in the region." [3]
Since late September, international donors have pledged more to the Ebola response than has been officially requested by international leaders. Actual disbursement of funds, however, still lags behind the total amount requested.” [3] [4] However, many pledges of international assistance did not make it to affected communities in a timely manner. “As of 31 December 2014, donors had pledged a total of $2.89bn to support the international response to the Ebola outbreak; however, only $1.09bn has actually been paid. ... It took until at least mid-October before the affected countries received $500m and until at least December before they got $1bn.” [6] Moreover, the appropriate skills and personnel were also not always available on the ground. This included doctors and nurses, as well as a lack of WHO operational personnel. [5]
Management
The WHO has a sound management structure with three levels of organisation: headquarters and regional and national offices. There was also a sub-regional operations coordinating centre to streamline the efforts of the WHO: the Sub-regional Operations Coordinating Centre (SEOCC) located in Conakry, Guinea. The SEOCC was the main operations hub for West Africa and served as a coordinating platform bringing together WHO and its partners to consolidate, harmonise, and streamline the technical support to affected countries. “The WHO and the Regional Office for Africa will coordinate international and regional deployments and activities, respectively, and will provide surge capacity to the SEOCC." [3] Each of the countries managed the Ebola response through a national task force or committee. However, stakeholders have criticised the WHO for not playing a coordinating role as it should. [5]Measurement
The WHO published regular weekly status report updates on Ebola case incidence and response activities.Data reported included the total cases suspected, probable and confirmed and the number of deaths. The status reports also reported capacity levels in the three affected countries to respond to Ebola and tracked progress made against target set out by the UN Missions for Ebola Emergency Response, such as isolating and treating Ebola cases and safely burying Ebola-related deaths. [8]Alignment
Despite an initial delay in taking action and poor coordination from the WHO early on during the breakout , the main actors collaborated to eradicate the epidemic, including the national governments affected, the WHO regional centres and the WHO headquarters. The WHO also partnered with agencies like United Nations Children's Fund (UNICEF), Centers for Disease Control and Prevention (CDC) and Médecins Sans Frontières (MSF) to provide clinical and public health interventions.
The WHO also provided technical, normative, material and operational support to the relevant ministries of the three main affected nations. “In accordance with the International Health Regulations (IHR 2005), the Ministries of Health of Guinea, Liberia, and Sierra Leone, together with WHO and other partners, are implementing a coordinated response to the outbreak." [3]
The International Development Association (IDA) and the International Finance Corporation (IFC) cooperated with the World Bank to fund the medical response and support the economies of the three countries mainly affected, which suffered significant downturns in economic activity as a result of EVD. [1]
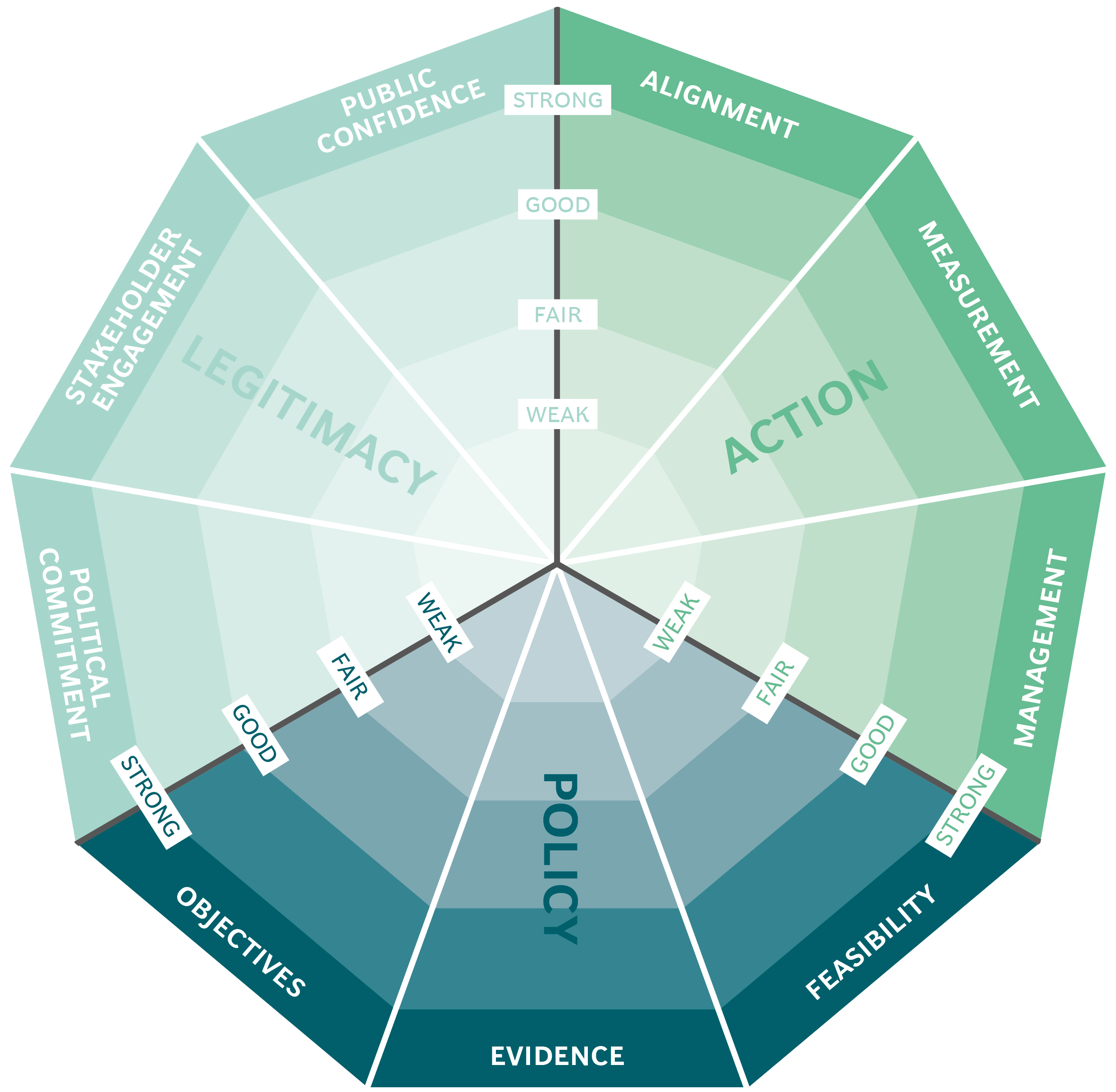
The Public Impact Fundamentals - A framework for successful policy
This case study has been assessed using the Public Impact Fundamentals, a simple framework and practical tool to help you assess your public policies and ensure the three fundamentals - Legitimacy, Policy and Action are embedded in them.
Learn more about the Fundamentals and how you can use them to access your own policies and initiatives.
You may also be interested in...


Organ Donations in Iran

Legislating to encourage organ donation in Israel

GAVI, the vaccine alliance

WHO: delivering insecticide treated nets to control malaria
