
National programmes for tackling dementia care in The Netherlands
The initiative
Alzheimer Nederland (the Dutch Alzheimer Society) initiated and participated in a national programme to improve dementia care: the National Dementia Programme [Landelijk Dementie Programma] (LDP), a four-year programme from 2004 to 2007. "Alzheimer Nederland coordinated with the Ministry of Public Health, Welfare and Sport and the Netherlands Institute for Care and Welfare (Vilans) a programme for regional providers of care, welfare and the treatment of dementia to improve dementia care from a client's perspective.”[2]
The main aim of the policymakers was to make community dementia care more complete and coherent in the Netherlands.
"In 2008, the policymakers introduced the Integrated Dementia Care Plan (2007-11) with the following objectives:
- "To design the range of coordinated dementia care options and the associated purchase of care ... to be available in practice throughout the Netherlands by 2011.
- "By the end of 2009 at the latest, dementia care best practices were to be available for all care providers involved...
- "To create some form of case management programmes which will form a part of the overall range of coordinated dementia care options by 2011.
- "To design the set of indicators for coordinated dementia care that would be in place nationwide by 2010 at the latest."[3]
Then in 2013, the government and policymakers introduced the "Delta plan" with the following objectives:
- "To provide proper care to 260,000 people with dementia living in the Netherlands.
- "To develop new concepts, services and products that allow people with dementia to be active participants in society for as long as possible."[4]
The challenge
According to the Netherlands Institute for Social Research (Sociaal Cultureel Planbureau, SCP), in 2009 there were on average three people involved in caring for a dementia sufferer. As there are over 260,000 dementia sufferers, "this means that there are currently more than one million people dealing with dementia in the Netherlands". [1]The public impact
The programme has been generally beneficial to carers. "In the period April 2006 - January 2007, the National Dementia Programme questionnaire was completed by 984 informal caregivers. Almost all informal caregivers (92.6%) received some professional support. However, two thirds (67.4%) indicated they had one or more needs for additional professional support. Informal caregivers often need additional professional advice about what to do when their relative is frightened, angry or confused."[5]
The dementia strategies have also been found to be useful. “Research has given us important tools to help today's patient and his/her carer. Cognitive training and adaption of the patient's living surroundings to their needs and wishes can improve quality of life and reduce behavioural problems.” This is according to the director of the Radboud Alzheimer Centre in Nijmegen and chair of Interdem, Professor Myrra Vernooij-Dassen.[6]
The Delta plan has been popular in that "90% of the country participated with 206 improvement projects fitting the needs of patients and families in the designing of Delta plan in 2013."[7]
Some the results published by Vilans in 2011 indicated significant public impact:
- "The number of regional networks is increasing
- "Dementia care is gaining importance, and higher decision-makers become involved
- "Indicators show that the degree of integration is increasing (stakeholders in regional dementia care co-operate ever more i.e. from 1.86 points on a 5-point scale in 2010 to 2.41 in 2011)
- "Availability of case management is increasing (from 2.13 points to 2.54 points) - patients and caregivers experience results of improved care (from 2.00 to 2.41)."[8]
Stakeholder engagement
There were many players (internal and external stakeholders) such as Vilans, the Dutch Institute of Healthcare Improvement, the Netherlands Institute for Social Research, care providers, and welfare and treatment providers. Alzheimer Nederland played a crucial role in the programme:
- "Providers of care, welfare and treatment worked together with volunteers from the Alzheimer Nederland...
- "Alzheimer Nederland and the national umbrella organisation of medical university hospitals... took the initiative for a new national plan. The new national plan is called the 'Delta Plan Dementia'. The name 'Delta Plan' was chosen as it reflects the increase in the numbers of people with dementia in a similar way to the expected flood of 1953. After the flood, a national strategy was formed to fight a possible new flood.[9]
- "Alzheimer Nederland and the municipalities under the Social Support Act would play a crucial role in policy development for early detection."[10]
- The Delta Plan is implemented by a public/private partnership including the government, the Alzheimer Centre and Alzheimer Nederland representing the public sector together with private companies such as Philips and Rabobank.
Political commitment
The Dutch government along with other stakeholders took the initiative to develop a dementia programme. The Dutch National Dementia Programme was launched and evaluated by the Dutch government. In 2013, the Delta plan was introduced by the government. which also cofinanced the Delta plan. "The Netherlands Dementia Delta Plan was launched today by the Minister for Health, Welfare and Sport Edith Schippers and Secretary of State Martin van Rijn... The Delta plan will invest 32.5 million euros over the next four years for scientific research into dementia."[10]Public confidence
It was estimated that 90% of the country's regions participated in the design of the Delta plan. Individual projects within the plan, such as Hogeweyk, were very popular with the public: “the cost of Hogeweyk is USD8,000 per month, but families never pay more than USD3,600 per resident, thanks to government subsidization. At the time this special was made, Dementia Village had a waiting list of 82.”[11]Clarity of objectives
The main goal defined at the programme's outset was clear and consistent: to make community dementia care more complete and coherent. There were different plans launched at regular intervals of time with a few changes along the way, for example the launch of the Delta plan in 2013.
There were subsidiary objectives, such as developing a set of indicators to monitor the growth of the project. "The information is gathered on the basis of a set of 35 indicators subdivided into ten themes. Much of the information measured is generic (i.e. not illness-specific). Coordinated care is one of the ten themes listed."[12]
Strength of evidence
The policymakers took several surveys to evaluate the project. Apart from this, the results and analysis of the surveys were shared with the stakeholders and then implemented in the strategy. “The LPD has 'compiled a national league table of the top 5 problem areas'. A second survey was carried out by Alzheimer Nederland. Alzheimer Nederland made the regional, data available to the regions concerned in February 2009. A second national analysis published in June 2009.” [13]
A significant component of evidence-gathering was to develop surveys, such as the LDP Monitor. "The survey of the most important problems was produced together with client panels of informal carers and using a special questionnaire based on the 14 problem areas: the LDP Monitor. In the LDP Monitor questions were asked concerning, on the one hand, the importance assigned to a 'problem area' by informal careers and, on the other, whether informal careers also experience problems within a problem area themselves.” [14]
Feasibility
There is no information for financial and legal feasibility. However, the policymakers estimated the requirements of professionals and other staff required to make the change happen. “The report by the Health Council of the Netherlands provides predictions of the size of the total population compared with the number of people suffering from dementia. This tells us something about the scope and potential of informal care. But also something about whether it is possible to provide sufficient numbers of professionals to deliver the necessary care.” [15]Management
The policymakers developed a proper mechanism to manage the policy. They launched their plans at regular intervals. Also there were skilled managers (LDP experts, client panels, General Practioners, etc) who have been executing the project. "The LDP expert team and professional dementia guidelines state that dementia diagnosis and support must always be linked. In practice this means that a permanent care provider should be available the moment the diagnosis is made. Naturally, the client will decide whether they wish to take up this offer (now or later). If need be. the case manager can always be called in at an earlier stage at the GP's request (at the stage when the patient feels that something is not right)."[16]
There was a special team formed to manage and monitor the progress. "The National Top 5 was compiled from the results of the client panels and ... analyses based on the LDP Monitor. The national analysis of 984 questionnaires and 700 members of client panels revealed that all 14 problem areas were sufficiently important and relevant to informal careers of people with dementia, and that the 14 problem areas do indeed coincide with the problems, obstacles and wishes of informal careers.”[17]
The Delta plan is very professionally managed and monitored (see Measurement below).
Measurement
The policymakers have monitored the progress of the programme on a regular basis. Policymakers used 35 different kinds of indicators (divided into 10 themes) to map the progress. For example care, communication and information, physical wellbeing, care-related safety, living and life circumstances were used (see Management above re the LDP Monitor).
Apart from this, indicators and surveys were used to meet the objectives of the policy. “Alzheimer Nederland collected the wishes and demands of families of patients in 160 focus groups and by means of a survey among caregivers.”[18]
Monitoring of the Delta plan is carefully carried out. “Each element of the Delta Plan has a separate project plan and will be organised by the participants in the way which seems best. Each element will be led by a project leader who will be appointed by a steering group. Progress is monitored by the steering group on a monthly basis.” [19]
Alignment
There is a strong alignment of interest between all the actors. All the stakeholders such as Alzheimer Nederland, National Association of General Practitioners cooperated effectively and executed their part. Alzheimer Nederland played a crucial role not only in the first and second programmes (2004-2007 and 2008-2011) but also in designing the Delta plan in 2013. "Alzheimer Nederland formed a broad alliance of public and private parties. Umbrella organisations are informed on a regular basis and will be involved in setting up the research programme and developing the e-health platform and national registry."[20]
Apart from this, private players such Nutricia, Philips and Rabobank were involved in the public-private partnership initiative to make the change happen.
Bibliography
Guideline for Integrated Dementia Care: An aid for the development of integrated dementia care, Revised May 2009, The Ministry of Health, Welfare and Sport
(https://www.alz.co.uk/sites/default/files/plans/netherlands.pdf)
National Alzheimer and Dementia Plans Planned Policies and Activities: Early Detection, Access to Diagnosis, and Stigma Reduction, April 2012, Alzheimer's Disease International
(https://www.alz.co.uk/sites/default/files/national-alzheimer-and-dementia-plans.pdf)
National Dementia Plan launched in The Netherlands, 4 April 2013, JPND Research
(http://www.neurodegenerationresearch.eu/2013/04/national-dementia-plan-launched-in-the-netherlands/)
National Dementia Strategies (diagnosis, treatment and research): Background information about the National Dementia Strategy, 2012, Alzheimer Europe
(http://www.alzheimer-europe.org/Policy-in-Practice2/Country-comparisons/2012-National-Dementia-Strategies-diagnosis-treatment-and-research/Netherlands)
National Programme for Dementia Care, 2011, Vilans
(http://www.moderne-dementiezorg.nl/upl/organisatie_van_zorg/2_VILANS_Poster_Dementia.pdf)
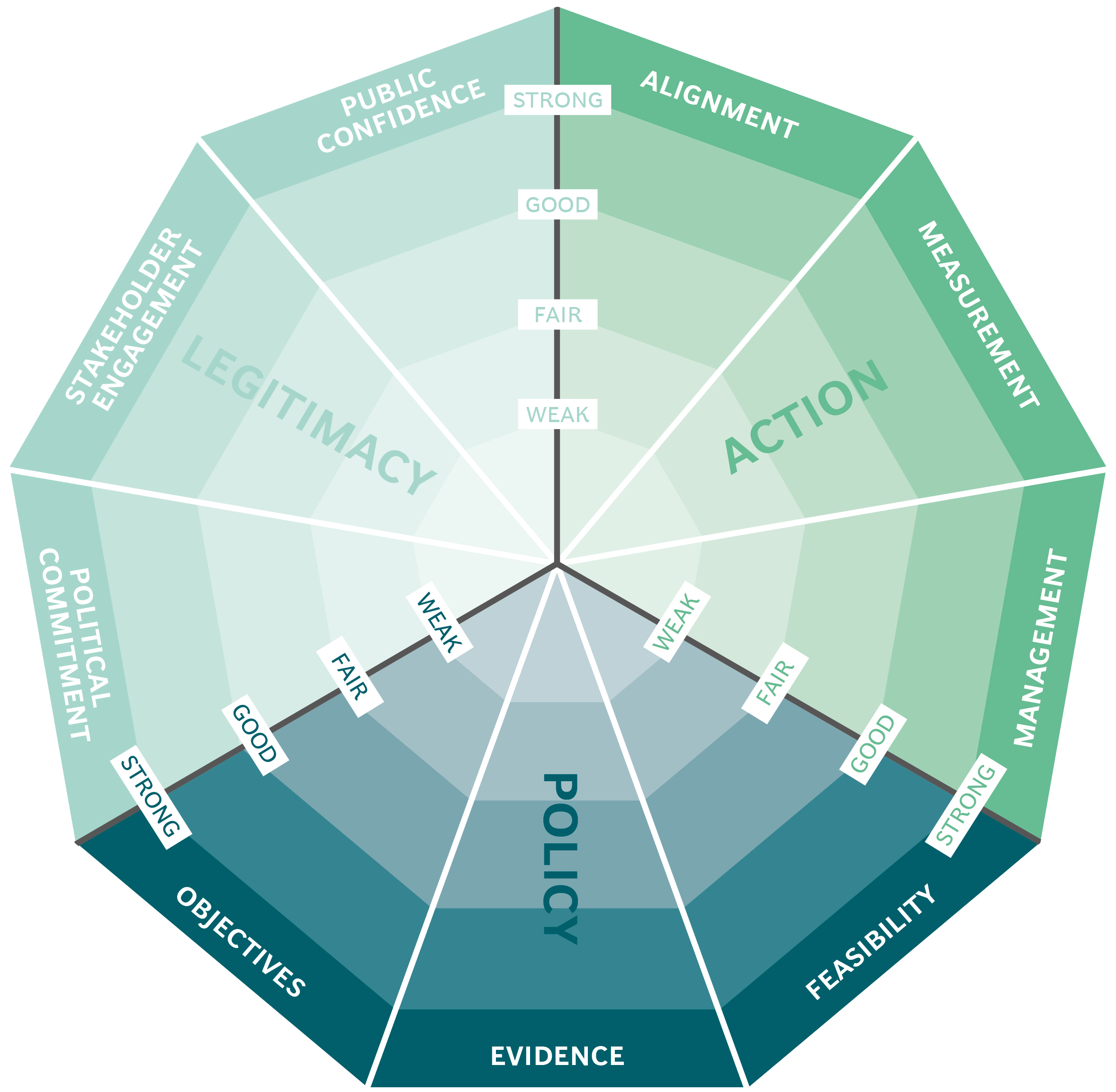
The Public Impact Fundamentals - A framework for successful policy
This case study has been assessed using the Public Impact Fundamentals, a simple framework and practical tool to help you assess your public policies and ensure the three fundamentals - Legitimacy, Policy and Action are embedded in them.
Learn more about the Fundamentals and how you can use them to access your own policies and initiatives.
You may also be interested in...


Organ Donations in Iran

Legislating to encourage organ donation in Israel

GAVI, the vaccine alliance

WHO: delivering insecticide treated nets to control malaria
