
Shine 2012: optimising medicine use for care home residents in Northumbria
The initiative
One response to these findings came from the Northumbria Healthcare NHS Foundation Trust supported by the charities Age UK and the Health Foundation, was the SHINE 2012 project. The lead clinician was Dr Wasim Baqir, a research and development pharmacist, and the project was defined as “a clinico-ethical framework for multidisciplinary review of medication in nursing homes”. Its starting premise was to propose “an innovative care home medication review service where residents and their families are involved in decisions about medicines”. [3]
The project's objectives were “to undertake detailed care home medication reviews, questioning the appropriateness of prescribing and ensuring that all medicines prescribed have a clear and documented indication, are safe and clinically beneficial”. [4]
The challenge
The use of medicines by the residents of care homes has been identified as an area of concern by a 2011 Health Foundation and Age UK report, ‘Making Care Safer'. The main issues it identified were:
- Communication and information sharing - standards of communication with carers were generally poor or inconsistent.
- Prescribing and administration of medication - residents' relatives “said they were ‘shocked but not surprised' by the high level of medication errors identified in care homes and provided several serious examples”. [1]
- staff development and support - low-skilled and unmotivated staff were identified as a key issue
- advocacy and rights - “care home staff often felt they needed to respect and protect the confidentiality of the resident, at the expense of sharing information with relatives. This sometimes prevented carers being given important information about changes in a resident's condition or medication.” [2]
The public impact
SHINE 2012 carried out 422 reviews carried out in 20 care homes in Northumbria. Its main impact was to:
- Make 1,346 interventions, most of which involved stopping the prescription or consumption of medication.
- Averaging 1.7 medicines stopped for every resident reviewed. The main reasons for stopping medicines were “no current indication” or “resident requested to stop”.
- Making net annualised savings of £77,703, or £184 per resident whose case was reviewed.
These had a beneficial effect, in terms of the residents' health and wellbeing, their carers' workload and their relatives' peace of mind.
Stakeholder engagement
The main institutional stakeholders of Shine 2012 were the Northumbria NHS Foundation Trust, Age UK Tyneside and the Health Foundation. The external stakeholders were the care homes, their managers, staff and residents - resident involvement was a key part of the project - and the residents' family members.
The Trust was fully engaged with both of its Clinical Commissioning Groups (CCGs) - North and South Tyneside. It worked with a number of charities other than the main stakeholders, e.g., Care Alliance and the consumer charity Healthwatch.
The project's observers were the Department of Health (DH), the Home Office (HO), Public Health England, The Royal College of Psychiatrists, The Royal College of General Practitioners, The British Psychological Society and the British Association of Sexual Health and HIV.
Political commitment
There is considerable, although complex, government support of the NHS and individual NHS Foundation Trusts, semi-autonomous units within the NHS, overseen by the DH. The DH and the HO are important government departments and were involved in the observation of Shine 2012. The DH is committed to any medically justifiable initiatives that may result in cost-savings.Public confidence
There is a generally high level of public support for the NHS and similarly for citizens' local NHS trusts, which is only compromised by demonstrably poor performance, as with the North Staffordshire NHS Foundation Trust, for example. An Ipsos MORI poll conducted in May 2012 found that:
- At national level, “69% of people are satisfied with the current running of the National Health Service (NHS). This matches the level of satisfaction recorded in December 2011 (70%) ... [5]
- “High levels of satisfaction are being maintained at a local level (75% agree their local NHS provides them a good service) and among service users (71% satisfied).”
Clarity of objectives
As stated in the Shine 2012 report, the aim of the project was to undertake a detailed review of the prescription and delivery of medication to care home residents and to intervene where any unnecessary or incorrect medication was prescribed and where carers were not carrying out the delivery of medicines to residents correctly. [6]Strength of evidence
The 2011 Health Foundation and Age UK report very clearly indicated that projects such as Shine 2012 was absolutely necessary. There were clear failings in care homes, both on the part of the carers and managers of the homes and the doctors who visited the residents as their patients.
The Shine 2012's approach was carefully thought out in order to test its proposals. It was itself a pilot project (of six months' duration). “The findings from the reviews were discussed within a multidisciplinary team (MDT). This project tested efficient ways of running an MDT and concluded that the core members needed to be the pharmacist and the care home nurse. Four models of general practitioner (GP) involvement (from no GP to GP attending the MDT), and two models of resident involvement (after and during the MDT) were tested.” [7]
Feasibility
Shine 2012 was adequately funded, principally by the Health Foundation. It was properly staffed, by experienced clinicians and researchers, who were qualified to recommend the medical interventions that formed an important part of the project. The project had an adequate reach to support its findings, in the number of care homes (20) and residents (422) visited and interviewed.Management
The lead clinician “The personnel involved in delivering [the] Shine project were the pharmacist, care home nurse, the GP, psychiatry of old age service (POAS) team (consultant and nurses) and the resident and/or their family or advocate.” [8] The lead clinician, Dr Wasim Baqir, is a senior clinical pharmacist with responsibility for research and development and managing the Trust’s pharmacy preregistration programme. The other members of the project were also well qualified. The POAS involvement was scaled down from the initial expectations.Measurement
Reviews were undertaken in the care homes by leveraging various sources such as GP records and data collection forms, after which any changes were recorded in GP clinical notes, care home records and the Shine 2012 database.
The scope of the investigation was sound as was the the quality of the data recorded. “Reviews were undertaken at 12 main care homes (fully reviewed) and 8 additional care homes (partially reviewed). The majority ... were mixed nursing and residential homes, with 3 being residential and 2 nursing only. Quantitative data were collected prospectively and entered onto our database at the end of each care home review. Our primary data sources were GP records, data collection forms (completed at the MDT), care home records (medicine administration record (MAR) and nursing notes. ... Changes resulting from the review are documented in triplicate: GP clinical notes, care home and our database. Data on medicines rounds pre- and post-Shine was collected from 8 care homes. Medicines waste data was collected from the community pharmacy supplying the homes; these data were date and quantity returned.” [9]
Alignment
There was a clear sense of cooperation with the care homes and their staff. ‘“To describe the Shine project I would say it was the best thing ever that ever that came into a care home. It looks at the individual and encourages them to feel part of any decisions' Care home manager.” [10] It also collaborated well residents and their family members: ‘““He explained things in layman terms. [The] pharmacist couldn't tell us to take her (mum) off the medication but he told us the pros and the cons and it was our decision and at least we were able to make an informed decision from the information from the pharmacist”. [11]
The Health Foundation funded Shine 2012 and there was a clear alignment of interests between them and Age UK, who partnered on the 2011 report, and between them and the Trust on the Shine 2012 project and report (which was published in 2014).
The Trust cooperated with other stakeholders and interested parties. “Working with the charity Care Alliance, Wasim Baqir, Aileen Beatty, Julian Hughes and Jo Mackintosh ran a ‘knowledge café' with staff from care homes in North Tyneside. We have been keeping GPs and other interested parties updated of our progress with coverage in the Trust's newsletter and social media (Facebook and Twitter). We presented the Shine project at the Royal Pharmaceutical Society (RPS) conference in September 2013, which is the UK's national Pharmacy conference. A report with early results (October 2013) was uploaded onto the RPS's Map of Evidence, a national repository of pharmacy quality improvement projects, audit and practice research.”
Bibliography
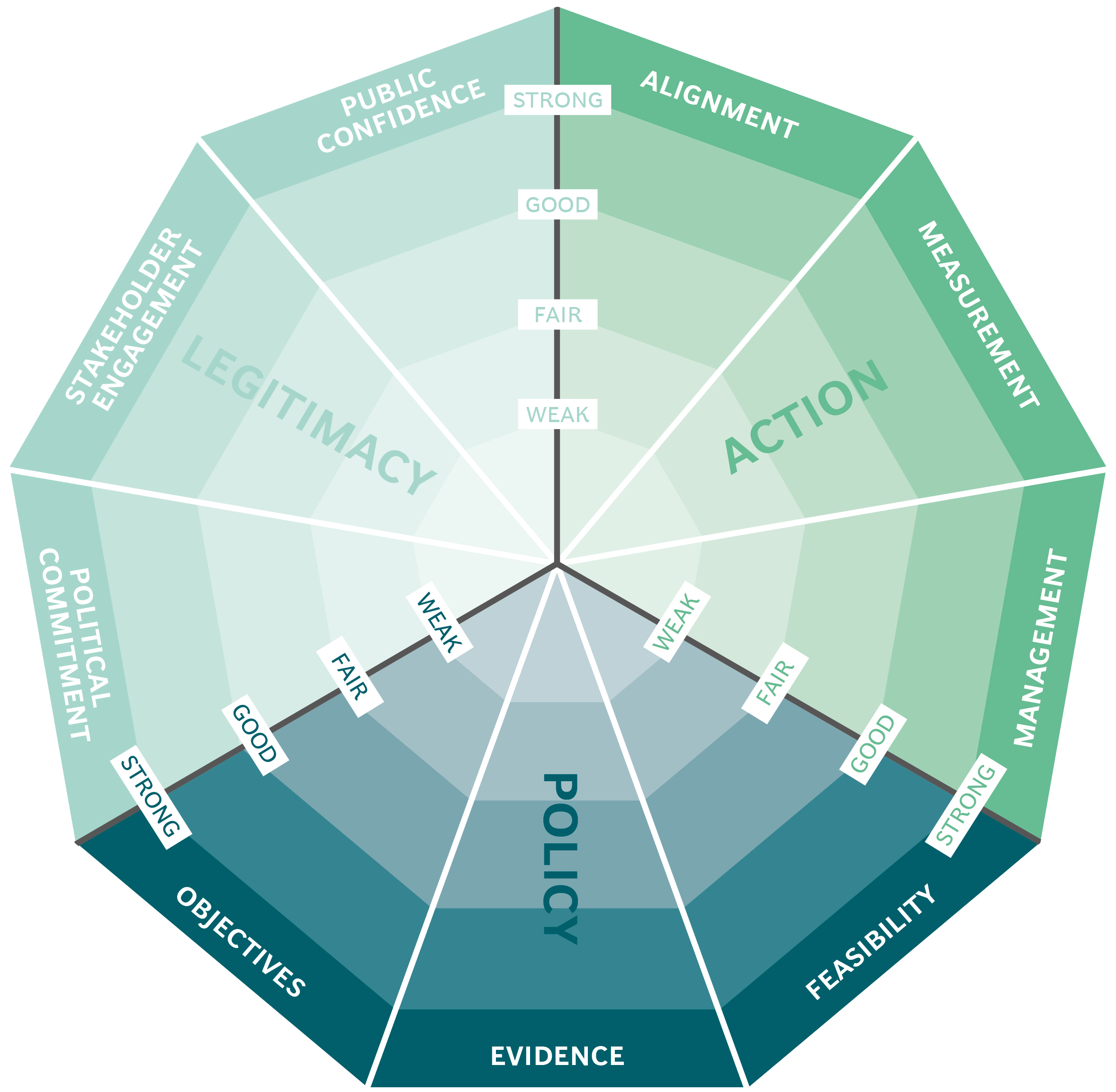
The Public Impact Fundamentals - A framework for successful policy
This case study has been assessed using the Public Impact Fundamentals, a simple framework and practical tool to help you assess your public policies and ensure the three fundamentals - Legitimacy, Policy and Action are embedded in them.
Learn more about the Fundamentals and how you can use them to access your own policies and initiatives.
You may also be interested in...


Organ Donations in Iran

Legislating to encourage organ donation in Israel

GAVI, the vaccine alliance

WHO: delivering insecticide treated nets to control malaria
