
National Tuberculosis Control Programme
The initiative
In response, the Revised National TB Control Programme (RNTCP), which applied the WHO-recommended strategy of Directly Observed Treatment Short course (DOTS), was launched in March 1997. The RNTCP was “expanded across the country in a phased manner. Full nationwide coverage was achieved in March 2006”. [1]
The goal of the programme is “to decrease mortality and morbidity due to TB and cut transmission of infection until TB ceases to be a major public health problem in India. The twin objectives of the RNTCP were to achieve and maintain a cure rate of at least 85 percent among new sputum positive (NSP) patients, and to achieve and maintain case detection of at least 70 percent of the estimated NSP cases in the community”. [2]
The challenge
Tuberculosis (TB) is a major health problem in India. It accounts for one-fifth of all global TB incidence and is estimated to have the highest number of active TB cases of any country in the world. The Indian National Tuberculosis Control Programme (NTCP) was set up in 1962 to control and eliminate TB, but it failed to achieve either goal.
When, in 1993, the World Health Organization (WHO) declared TB to be a global emergency, it was clearly time for the Indian government to step up its anti-TB activities.
The public impact
Since its inception, the RNTCP has caused over 13.8 million patients to be placed on treatment, thus saving more than 2.5 million additional lives as compared to NCTP.
The overall performance of the RNTCP has been very good. The cure/treatment completion rate has been consistently above the 85 percent target, and the death rate among registered patients has been reduced to less than five percent. More than 90 percent of NSP patients are now being given a DOTS course. “As a result of the implementation of RNTCP in the country, prevalence of all forms of TB has been brought down from 338 per 100,000 population (1990) to 249 per 100,000 population in 2009 and TB mortality in the country has reduced from over 42 per 100,000 population in 1990 to 23 per 100,000 population in 2009, as per the WHO global TB report 2010.” [3]
Stakeholder engagement
The RNTCP has a number of stakeholders, principally the federal and state governments – led by the Ministry of Health – the medical profession, TB patients and the WHO. “More than 3,000 NGOs, 30,000 private practitioners and 150 corporate health facilities are involved in the provision of RNTCP services. [Nearly 300] medical colleges have been involved ... [as have] health facilities in government sectors viz. Employees State Insurance, railways, ports and the Ministries of Mines, Steel, Coal, etc. Intensified PPM activities are being undertaken with the Indian Medical Association (IMA) in 16 states and with the Catholic Bishop Conference of India.” [4]Political commitment
The Indian government funded the programme and played an important role in distributing the medicines. “Free Anti-TB drugs are being received from Govt. Medical Store Depots on a quarterly basis against release orders by the Central TB Division.” [5]
Under Global Funding for AIDS, TB and Malaria, an Indian government project, the IMA in Punjab, has initiated a public-private partnership project between the IMA, the state of Punjab and the RNTCP. This is an example of a state-level initiative, which is indicative of state governments' steps to eliminate TB.
Public confidence
The Indian public are generally unhappy with the health facilities that the government has been providing, particularly in hospitals. However, this does not apply specifically to its anti-TB programmes.
Public opinion about government health services has been analysed in the light of violence in hospitals and subsequent strikes by medical staff. “Patients were angry that doctors had gone on strike ... The most common grievance of patients was the hospital staff's rude behaviour ... Patients were also angry about the constant demands to pay for services or to purchase materials from outside. Other major grievances were delays, being shuttled from department to department and poor communication about the patient's condition.” [6]
Clarity of objectives
As stated above (in The initiative), the RNTCP’s broad objectives were to reduce mortality and morbidity due to TB and to reduce the transmission of infection. [7] The detailed and quantifiable objectives were a cure rate of at least 85 percent and case detection of at least 70 percent. These were clear and were in fact met.Strength of evidence
Policymakers gathered evidence from the pilot phases that were conducted in 1993 and also a number of surveys to gather the relevant evidence during the subsequent phase. The RNTCP “was started in India in 1993 as a pilot strategy (Phase-I) at five places in the country and it could achieve a cure rate of more than 90 percent. Encouraged by these results, the strategy was extended to cover 14 million [people] in order to study technical soundness and operational feasibility of RNTCP in phase-II”. [8]
For example, “repeat population surveys ... in Chengleput, Tamil Nadu indicated that since RNTCP implementation a 12 percent annual decline in prevalence has occurred, much greater than the decline observed in the preceding decades in the same area”. [9]
Feasibility
The technical feasibility was established by the 1993 pilot project and is reinforced by the involvement of the WHO. The financial feasibility was addressed by funding from the WHO and the federal government, which supported the state governments in their local RNTCP initiatives.Management
The RNTCP is being managed by the Indian government through the Ministry of Health. The Central Tuberculosis Division under the supervision of Directorate of Health Services manages the RNTCP programme.
It applies the WHO's DOTS strategy, which has five components, each one of which is part of a management package provided by WHO. “The components of DOTS are: (i) political and administrative commitment; (ii) good quality diagnosis, (iii) good quality drugs, (iv) the right treatment, given in the right way; and (v) systematic monitoring and accountability.” [10]
In addition, “enhanced supervision is ensured through a ‘Tuberculosis Unit', a sub-district level unit comprising of specialized staff”. [11]
Measurement
There were different mechanisms to measure and monitor the success of the RNTCP: surveys, evaluation strategies and a use of cohort analysis of the treatment results. A health information network was constantly monitoring the progress of the programme. The WHO used mathematical modelling techniques to estimate the impact.
Combatting TB was part of the UN's sixth Millennium Development Goal, specifically to reverse TB incidence by 2015. “The Programme has initiated surveys to assess the impact of RNTCP and progress towards TB related millennium developmental goals. These include: Disease prevalence surveys at seven sentinel sites and the National annual risk of TB infection survey. The results of these surveys will be used to realistically estimate the disease burden in the country in consultation with both national and international technical experts.” [12]
Alignment
All the actors, such as the Ministry of Health, the IMA and the WHO shared a common goal of eradicating TB, and cooperated effectively in the RNTCP. There was evidence of collaboration at federal and at state level, for example in the Punjab, between the WHO, the IMA and the state government. There was general alignment between NGOs and medical practitioners throughout India.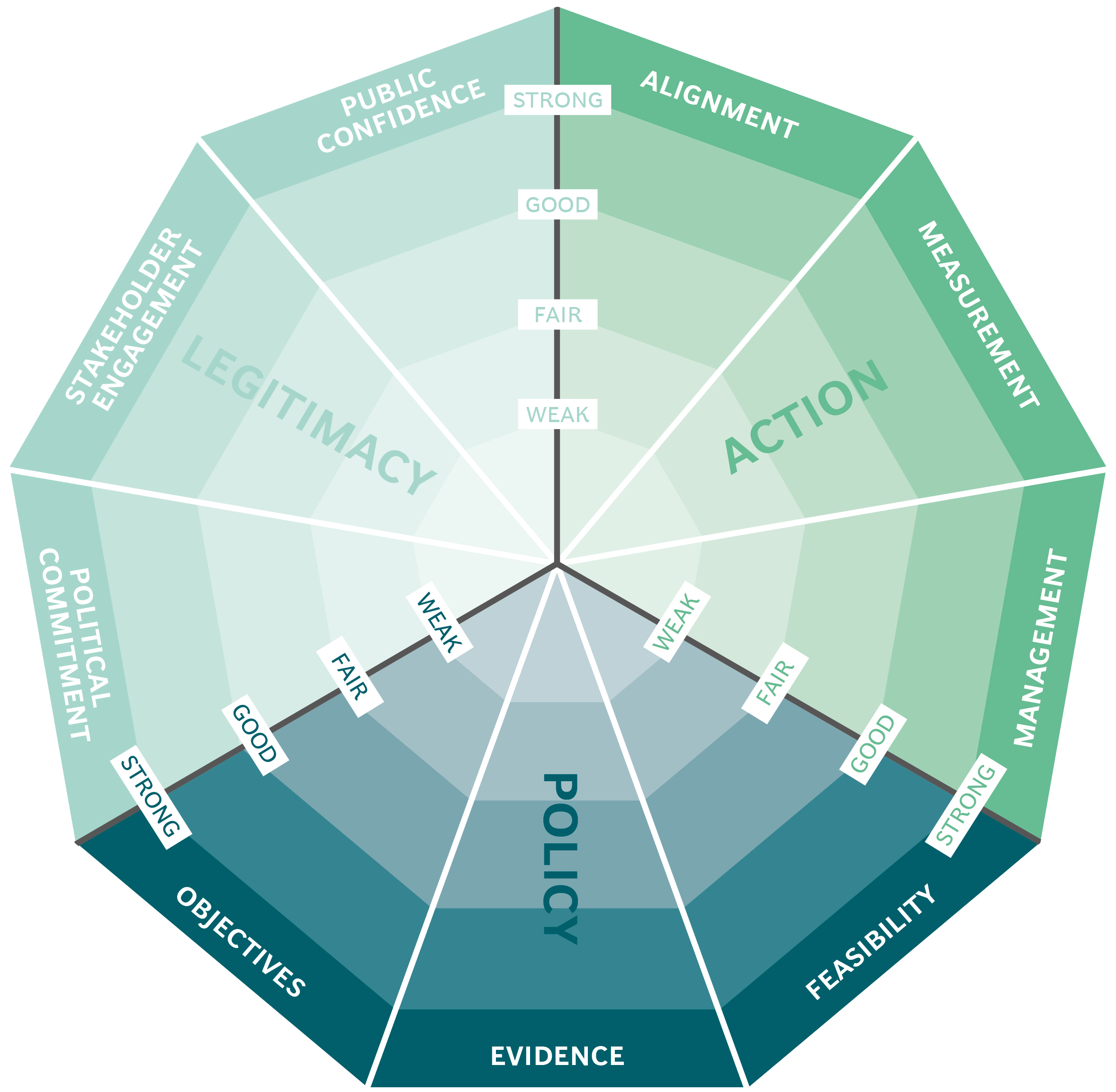
The Public Impact Fundamentals - A framework for successful policy
This case study has been assessed using the Public Impact Fundamentals, a simple framework and practical tool to help you assess your public policies and ensure the three fundamentals - Legitimacy, Policy and Action are embedded in them.
Learn more about the Fundamentals and how you can use them to access your own policies and initiatives.
You may also be interested in...


Organ Donations in Iran

Legislating to encourage organ donation in Israel

GAVI, the vaccine alliance

WHO: delivering insecticide treated nets to control malaria
