
The Australian National Bowel Cancer Screening Programme (NBCSP)
The initiative
Given that patients rarely present with obvious symptoms, there is a pressing need to screen those most at risk. In order to do this “the National Bowel Cancer Screening Program (NBCSP) was initiated by the Australian government in 2006, in partnership with state and territory governments, to help detect bowel cancer early and reduce the number of Australians who die each year from the disease”.[3]
The overarching goal of the NBCSP, which is still in operation, is “to reduce the morbidity and mortality from bowel cancer by actively recruiting and screening the target population for early detection or prevention of the disease”.[4]
The specific objectives, as set out in the National Bowel Cancer Screening Program Policy Framework Phase Three (July 2013-June 2017), include :
- “Achieving participation levels that maximise the population benefit of early detection of bowel cancer in the target population.
- “Enabling equitable access to the programme for men and women in the target population, irrespective of their geographic, socioeconomic, disability or cultural background ...
- “Facilitating the provision of timely, appropriate, high quality and safe diagnostic assessment services for programme participants …
- Collecting and analyse data to monitor participant outcomes and evaluate programme effectiveness.”
The process for all individuals who are enrolled in the NBCSP is relatively straightforward. “[He or she] collects a stool sample using the supplied kit and posts it to a nominated pathology laboratory for analysis. Results are sent to the participant, the participant's primary health care provider (PHCP) - their GP -and the NBCSP Register. Participants with a positive result, indicating blood in their stool, are advised to consult their PHCP to discuss further diagnostic testing - in most cases, this will be a colonoscopy. Responses to invitations, and the outcomes for participants who complete the screening test, are monitored to the point of definite diagnosis for those who are found to have bowel cancer.”[5]
The challenge
One of the most serious medical problems facing Australia is the high incidence of bowel cancer. “Australia has one of the highest rates of bowel cancer in the world. About one in 23 Australians will develop bowel cancer before their 75th birthday … Around 80 Australians die each week from bowel cancer, making it the second most common cause of cancer-related death after lung cancer ... The good news is that, if found early, 9 out of 10 cases of bowel cancer can be successfully treated.”[1] The difficulty lies in finding the disease early, as “most people diagnosed with bowel cancer have few, if any, symptoms)”.[2]The public impact
From the inception of the NBCSP in 2006 to 2014:
- “Over 2.5 million Australians were screened.
- “3, 989 people were found to have suspected or confirmed cancers.
- “12,294 people were diagnosed with advanced adenomas (benign tumours that may become cancerous).”[6]
A 2014 study (Analysis of bowel cancer outcomes for the National Bowel Cancer Screening Program by the Australian Institute for Health and Welfare, December 2014) “found that people who were invited to screen through the [NBCSP] had 15% less risk of dying from bowel cancer, and were more likely to have less-advanced bowel cancers when diagnosed, than people who were not invited”.[7]
Stakeholder engagement
The government is the key stakeholder. It has committed hundreds of millions of dollars to establishing and growing the NBCSP over the past ten years - first as a pilot programme and then as a fully-fledged initiative - and has maintained the NBCSP as a health policy priority.
Health professionals involved in the follow-up were highly engaged, both in carrying out follow up procedures (e.g., colonoscopies) and in promoting the NBCSP. “83 percent of GPs and 62 percent of colonoscopists surveyed having recommended participation in the NBCSP to patients.”[8] Health professionals are encouraged to engage using financial incentives.
There are a number of medical organisations among the stakeholders:
- The Cancer Council Australia, a national NGO working to reduce the impact of cancer in Australia, advertises the NBCSP on their website.
- “The test kits are manufactured by Japan-based Fujirebio Diagnostics, imported into Australia by Siemens Medical Healthcare Diagnostics.”[9]
- Medicare accurately maintains the register of test participation data and outcomes.
- The Gastroenterological Society of Australia lends experts to NBCSP policy boards and develops an improved training programme for colonoscopists.
Political commitment
The NBCSP was initiated during John Howard's time as coalition prime minister. Christopher Stevenson, who in 2006 was a Senior Analyst at the Australian Institute for Health and Welfare, noted the programme came about during election season. “The government was looking for things to support,” said Stevenson. “There had been a growing movement for Bowel Cancer Screening for some time. At the time, a number of randomized control trials had demonstrated that fecal testing was an effective way of reducing bowel cancer.” Stevenson noted that several prominent and respected colon rectal surgeons were lobbying for the programme, which put added pressure on the government to respond.
The programme has continued during two subsequent Labour governments, and the targets were raised under the current Liberal/National coalition. These actions indicate that the programme has strong support from all major political parties:
- “The Gillard government set aside AUD139 million over four years in the 2011 budget to continue the [NBCSP].”[10]
- “In the 2014 Federal Budget, the Coalition Government announced an additional AUD95.9 million over four years to accelerate implementation of the [NBCSP] to all Australians aged 50 to 74 years by 2020.”[11]
Public confidence
A 2008 study in the Medical Journal of Australia indicated that the majority of Australians are confident in doctors, Medicare and the public health system in Australia.
Public participation in this scheme is not yet at target levels: “of the 963,518 eligible people invited into the NBCSP in 2012-13, 321,413 (33.4%) had participated by 31 December 2013.”[12] However, this need not imply a lack of public confidence in the NBCSP, which may have been compromised by a batch of faulty test kits distributed in 2008 and perceptions of the accuracy of the test.
Although participation rates are still suboptimal, 2015 survey data suggests that Australians are confident in the programme, with a strong majority agreeing that the NBCSP “provides a high quality service [and] is effective at detecting cancer early."[13] From the start, Australia's economic and cultural diversity presented a challenge to participation. Stevenson pointed to different languages, beliefs, and attitudes about health among the groups. “There was a lot of work around getting the participation of indigenous groups because their response was ‘cancer is a disease of older people, and our people should be so lucky to get cancer if they live to such an age.'”
Clarity of objectives
The objectives are clear and measurable and have been retained throughout the NBCSP to date: to reduce morbidity and mortality rates from bowel cancer through a screening programme with high levels of participation from all areas of Australian society.Strength of evidence
The NBCSP was based on evidence from previous randomised controlled trials and a pilot screening programme in the UK: “in 1996, the Australian Health Technology Advisory Committee systematically reviewed the literature on screening for bowel cancer against the World Health Organization principles for the assessment of a screening programme.”[14]
Country-specific evidence was drawn from the 2002-2004 Australia Bowel Cancer Screening Pilot programme, which was conducted by the (now renamed) Australian Government Department of Health and Ageing in Melbourne, Mackay, and Adelaide. “The primary aim of the Pilot was to provide information about the feasibility, acceptability and cost effectiveness of bowel cancer screening amongst the Australian population in both rural and urban areas.”[15]
Feasibility
The feasibility was demonstrated in a number of areas:
- Financial - the government committed to significant and sufficient ongoing funding for the NBCSP. Although as the initial programme was a pilot, early funding was limited. “I recall the bureaucrat leading it telling us that we were not to look for a Rolls-Royce programme, this was more of a Gemini programme,” said Christopher Stevenson of the Australian Institute for Health and Welfare. Gemini was aninexpensive car manufactured in Australia. “We had to operate with some pretty strict resource constraints. Because resources were tight a lot of creative thinking went into how to do it in a way that minimized resources but was still a scientifically reliable thing to do.”
- HR - Australia already has a well-developed healthcare system, with skilled health professionals, e.g., GPs, colonoscopists and colorectal surgeons. The increased rate of screening put pressure on colonoscopy clinics, particularly in rural and remote areas. Services were “generally of good quality, but workforce capacity and capability varied between metropolitan, rural and remote regions”.[16]
Management
The NBCSP is administered by the Department of Health to the point of the FOBT result from the screening, where it is taken over by the states and territories. The Department of Health is responsible for NBCSP management and governance, policy development and funding.
States and territories have an advisory role for the NBCSP through the Screening Subcommittee of the Australian Population Health Development Principal Committee, as well as the NBCSP Programme Managers' Group and the NBCSP Programme Advisory Group (PAG). Clinicians are also represented on the PAG, whose role is to provide advice to the Department of Health on issues relating to the NBCSP.
A KPMG review of the programme in 2012 indicated that management was very professional. In terms of managing the service delivery components of the programme, the review concluded that the "distribution of kits, operation of the information line, analysis and reporting of results, and the mail house functions are all working effectively [as is] the Register.”[17]
Measurement
NBCSP has a comprehensive measurement function: “the NBCSP performance indicator set comprises 11 endorsed indicators that are used for monitoring the programme”.[18]
“Responses to invitations, and the outcomes for participants who complete the screening test, are monitored to the point of definite diagnosis for those who are found to have bowel cancer ... The AIHW produces these NBCSP monitoring reports for the Australian Government Department of Health. These reports analyse data extracted from the NBCSP Register and provide an overview of screening participation and outcomes.”[19]
Alignment
There was a great deal of positive cooperation between the medical profession and the Department of Health to ensure the success of the NBCSP.
GPs were already concerned about bowel cancer rates and recommended a screening programme. “The Royal Australian College of General Practitioners' guidelines for preventive medicine in general practice (‘the Red Book') also recommend regular screening for bowel cancer using FOBT for people aged over 50 years.”[20]
Bowel Cancer Australia, a community-funded charity that aims to increase awareness of bowel cancer and fund bowel cancer research, is also aligned with the NBCSP, and is working to provide access to the same screening tools for people who fall outside the national scheme's age bracket.
The Cancer Council Australia, a national NGO working to reduce the impact of cancer in Australia, is also aligned with the NBCSP in its goal of screening for early detection of the disease.
Bibliography
National Bowel Cancer Screening Program Policy Framework Phase Three, July 2013-June 2017, 30 May 2013, Endorsed by the Community Care and Population Health Principal Committee
Key statistics, National Bowel Cancer Screening Program, Department of Health
Performance indicators, National Bowel Cancer Screening Program, Department of Health
Self-Test Bowel Cancer Kits - Important Notice for Users, Department of Health
Interview to: Christopher Stevenson, Former Senior Analyst, Australian Institute for Health and Welfare (AHW)
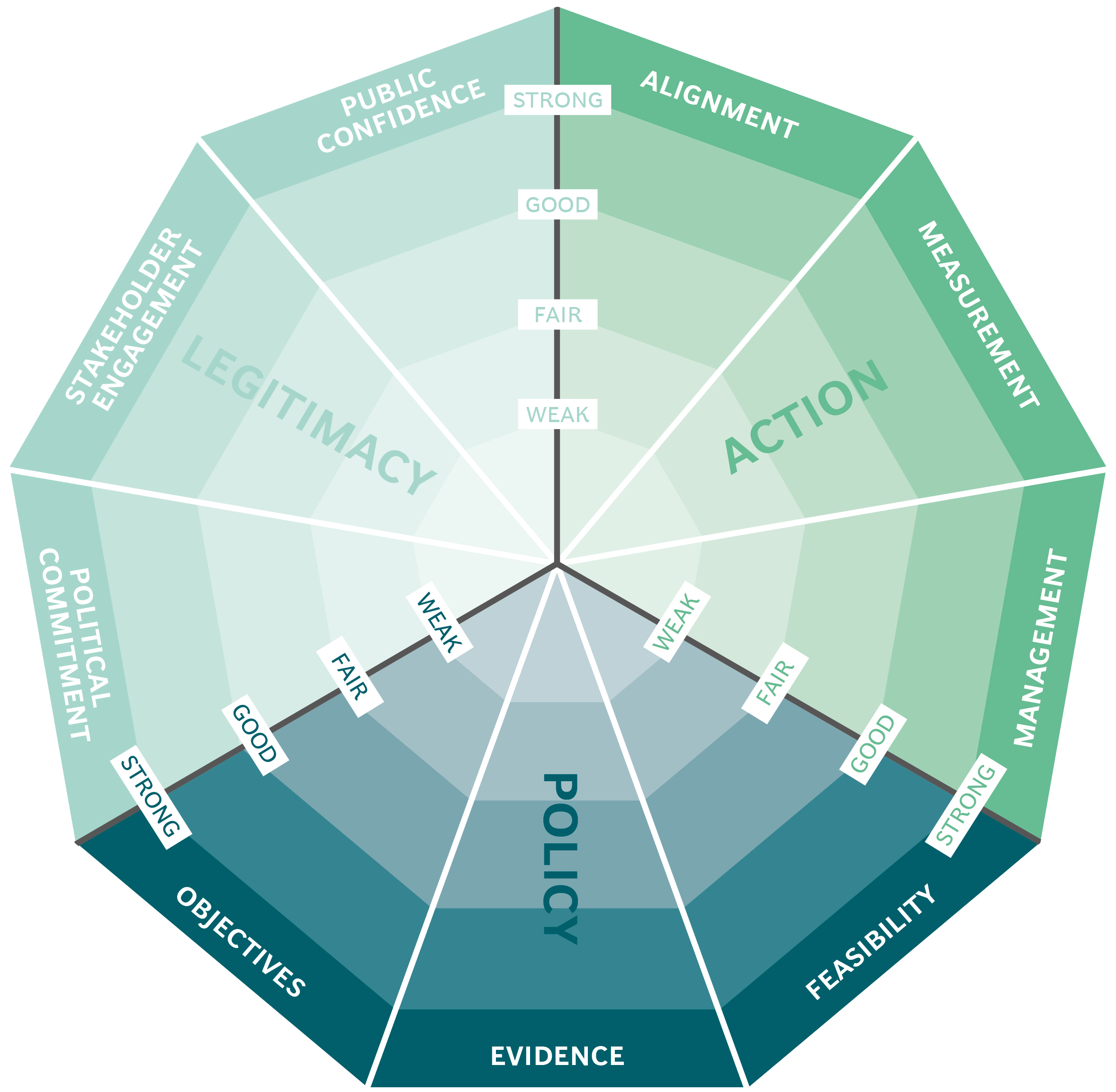
The Public Impact Fundamentals - A framework for successful policy
This case study has been assessed using the Public Impact Fundamentals, a simple framework and practical tool to help you assess your public policies and ensure the three fundamentals - Legitimacy, Policy and Action are embedded in them.
Learn more about the Fundamentals and how you can use them to access your own policies and initiatives.
You may also be interested in...


Organ Donations in Iran

Legislating to encourage organ donation in Israel

GAVI, the vaccine alliance

WHO: delivering insecticide treated nets to control malaria
