
Alaska’s Telehealth Solutions programme
In a state where people would just as often use a snowmobile, dogsled, boat or helicopter as a motor vehicle to get to a hospital, providing a functioning healthcare system for over 200,000 beneficiaries is challenging.[1] In Alaska, a shortage of healthcare professionals and the long distances between them and many of their patients exacerbates the problem. For Alaskans, telehealth - healthcare delivery using the transfer of medical data through audio, video or data communications - was an ideal solution.[2]
The 1998 Telehealth Solutions programme was rolled out over Alaska's extensive territory, providing doctors with the ability to monitor and follow up on patients remotely through mobile computers, and it has helped overcome the stark isolation of some of its villages. The telehealth programme has so far connected approximately 180 Alaska Native community village clinics, 25 subregional clinics, 4 multi-physician health centres, 6 regional hospitals, and the Alaska Native Medical Center (ANMC) in Anchorage, Alaska's most populous city.
The initiative
With the staff of most rural health facilities being unfamiliar with current and unfolding technology, as well as professional and beneficiary locations in isolated areas, the Alaska Federal Health Care Access Network (AFHCAN) started to explore opportunities for telehealth and seek to establish a statewide telehealth network. Telehealth has been defined as the “delivery of health-related services and information via telecommunication technologies”.[5]
The AFHCAN began to develop its IT-based telehealth programme in 1998, launching it in 1999, at which time it was the largest telehealth endeavour in the world,[4] providing Alaskans living in underserved rural areas with the tools to manage their own health.[1] The Telehealth Solutions programme comprises a home health monitoring programme and the establishment of an extensive videoconferencing system.
At the centre of the initiative are the AFHCAN's carts. “With painstaking attention to every detail, the AFHCAN created and deployed telemedicine ‘carts'—a combination of off-the-shelf hardware and specifically designed software, which utilised a web-based ‘store-and-forward' interface and data collection protocol.”[4] In many clinics, the cart is now the only computer being used. It is “a mobile telemedicine workstation equipped with a variety of measurement and monitoring devices to collect clinical data for both general and specialty care providers servicing rural health clinics. Each cart is tailored to the health needs and training of the rural clinic site. Thus, AFHCAN carts at different sites have different peripheral devices such as an audiometer, tympanometry, and video otoscope.”[5]
The clear advantage of this approach in the Alaskan context was that it did not require high bandwidth to send and receive data and hence could operate on basic phone networks. “Assuming telecommunication resources were available, rural and remote clinics with carts could be networked with larger healthcare centres, which could provide them and their patients with access to physicians and specialists from more populated areas.”[4]
The challenge
Alaska is the biggest state in the US but has the lowest population density, and is often called “America's last frontier”. Compared to other states when it comes to healthcare, Alaska faces unique challenges: its small population of around 710,000 is spread out over a challenging landscape, ranging from the rocky coast and Aleutian Islands to Denali's rugged interior to the Arctic Circle and numerous small, secluded islands - many Alaskan villages are only accessible by boat or bush plane.
The challenge for Alaska's healthcare providers is to deliver appropriate healthcare services to a population of over 200,000 beneficiaries, of whom 60 percent live outside the Anchorage area. The CIO of the Norton Sound Health Corporation (NSHC) in Nome, assesses the situation as follows: "When we talk about delivering healthcare in a land mass that's basically half the size of the lower continental United States of America, we're trying to do all these things using alternative methods to deliver that healthcare”.[3] The NHSC is a tribally-owned, independent, not-for-profit organisation providing healthcare in Alaska's Norton Sound region.
Alaska's “geographic barriers” lead to many other difficulties, such as the shortage of personnel and the higher costs of operating medical services within the state. Small villages in Alaska are often not connected to any road system and have no nurse practitioner in the community, let alone a hospital, doctor or specialist. Alaska has one of the lowest rates of medical specialists in the US, and 65 percent of all doctors are based in Anchorage. In the 1990s, most of Alaska's federally funded clinics and hospitals were understaffed and under-equipped, using 20-year-old medical technology and communication systems. They rely heavily on air transport for patients, physicians and medical supplies, while the weather is often unpredictable.[4]
Blue Cross has estimated that the general cost of operating a hospital or clinic is 300 percent more expensive in Alaska than in the continental US. Even though technology can help to overcome these challenges, “many rural clinics and healthcare facilities are neither familiar with nor using current and unfolding technology”.[4] Under these conditions, access to healthcare for Alaskans was very limited, and a change in the system was required.
The public impact
Since its establishment, the telehealth programme has connected approximately 180 Alaska Native community village clinics, 25 subregional clinics, 4 multi-physician health centres, 6 regional hospitals, and the ANMC in Anchorage. The clinics, health centres, and regional hospitals are operated by local health organisations or foundations and serve an average of 23,000 patients a year.[6] As of 2018, telemedicine is still widely in use and, in fact, has been further enhanced by a law that was put in place in 2016 by Alaska Governor Bill Walker. This legislation authorised the expansion of the use of telehealth to a wider array of clinical practices such as licensed audiologists, speech language pathologists, counsellors, marriage and family therapists, psychologists, and social workers.[7]
Evaluation data demonstrated that telemedicine using the AFHCAN's resources significantly increased rural and remote access to healthcare. “It facilitated referrer-physician communication, enhanced patient education, improved quality of care for patients, and increased satisfaction of both providers and patients.”[4] Besides these beneficial aspects, telehealth also meant huge cost-savings on medical flights, because patients' medical condition could be closely monitored with the help of mobile carts in rural health centres. For example, in a cardiac patient “who'd been transported by helicopter to a hospital five times one year, costing the system USD22,000 per flight and spending a total of 53 days in the hospital”, signs of stress could be picked up at an earlier stage while the patient was involved in her own care.[1] “Patients self-identify problems earlier, and it really provides a way for us to be more proactive in their management - and gets them involved as well,” said Samuel C. Johnson III, executive director of the Alaska Federal Healthcare Partnership (AFHCP).[1] The AFHCP is using a device that transmits patient data several times a day.
The AFHCAN Telehealth Solutions programme has recorded more than 100,000 telehealth encounters - leading to savings of more than USD6 million annually in travel and healthcare expenses. The AFHCP's Alaska Native Medical Center in Anchorage receives about 3,000 remote cases a year for telehealth consults, which have proved to be especially time-saving when it comes to children needing surgery to implant ear tubes,[4] and for performing lifesaving surgeries remotely. The Alaska Native Health Consortium estimated that 20 percent of Alaska Natives rely on telehealth, and that remote consultations within their network save USD10 million annually in travel costs. The consortium said that they “cannot provide care in rural Alaska without telecommunications”.[8]
In June 2003, for example, a new use of telemedicine technology helped save the life of a woman receiving care at Maniilaq Health Center in Kotzebue, in north-west Alaska. The woman came to the hospital with an ectopic pregnancy which had ruptured arterial blood vessels, so that she was haemorrhaging and her condition was deteriorating rapidly. She needed immediate surgery, but the Maniilaq Health Center had no operating room, surgeon or anaesthesia. “‘Due to heavy fog, there was no way we could medevac her to a larger facility with an operating room,' said Dr Michael Orms in Kotzebue. ‘There was a high possibility that she would have died even in transport to Anchorage... Being a family practitioner - but not a surgeon - I needed some assistance.' Dr Orms called the medical director at the Women's Health at the Anchorage Native Primary Care Center for guidance on how to do a laparotomy using local anaesthesia. AFHCAN staff set up a monitor and Kotzebue staff brought videoconferencing equipment into the room, so that the surgery could be observed from Anchorage while doctors of the PCC Women's clinic talked with Dr Orms on the telephone.”[4]
This example points to the possible benefits specialists can offer through telemedicine in support of doctors in remote sites under emergency conditions. However, due to the almost overwhelming complexity of designing, developing, and deploying a telehealth project of this scope in a state as large as Alaska, progress was somewhat slower than originally projected.[20] “The telehealth undertaking in Alaska was slow to start. Progress was stalled in getting equipment to the villages, physicians and health aides were slow to begin using the equipment, and in many locations the connectivity could not support the transfer of images.”[4] These problems were eventually overcome.
Written by Julia Schnatz
Stakeholder engagement
Long before the Alaskan government launched its Telehealth Solutions programme, several conferences were held to discuss ways and means for it to work. Regional Native health corporations were fully involved in the discussions and committed to the programme. The initial pilot for establishing a telemedicine network in Alaska was proposed by a consortium of healthcare providers, telecommunications companies, the University of Alaska, and interested private citizens, who had already been developing plans for such a programme.
The main component of the telehealth programme was to develop a care tool in the form of a medical cart. This primary care tool was designed by the Alaska Native Tribal Health Consortium (ANTHC) together with professionals from different specialisms in the Alaska Native Medical centre as well as the users on the ground - the nurses and health aides within the rural communities.[9] They developed the functions of the cart according to the users' requirements, e.g. cameras, microphones and data input surfaces were combined into one big desktop computer, which was then distributed to the remote tribal healthcare centres.
The main stakeholders in this process were the ANTHC, which had been led by Dr Stewart Ferguson since the inception of the initiative, and the Alaska Native Medical centre. They collaborated closely in developing the programme.
Healthcare providers and key players in the telehealth initiative, such as the rural clinics, considered the AFHCAN project to be successful, since it greatly improved access and quality of healthcare for otherwise isolated populations.[4]
Political commitment
Historically, there has been strong political commitment to the use of telecommunications in Alaska. The 1996 Telecommunications Act, which was passed by the federal government, stimulated new interest and activity in telemedicine deployment in remote areas in Alaska.
Telehealth has been an issue since the 1950s and, since then, many politicians - Democrats and Republicans alike - have been aware of the need for it, and have been supportive and willing to expend political capital to achieve it. In 2018, Alaskan senators, Lisa Murkowski and Dan Sullivan, joined a coalition of 30 US senators in calling on the Federal Communications Commission (FCC) to increase the Rural Health Care Program's spending cap. And the Trump Administration has broadly recognised the value of telemedicine, especially for veterans.[8]
Investment in the AFHCAN, which had been proposed by the Alaska Federal Health Care Partnership (AFHCP), was assured by the end of 1998 through the legislative and budgetary initiatives of Alaska's senior senator, Ted Stevens. He also initiated the formation of the Alaska Telehealth Advisory council, a body that consisted of the potential major players in telemedicine to inform the rollout of the telemedicine policy in Alaska.[4]
During the subsequent implementation phase, “state involvement was occurring through technical assistance from participation in AFHCAN by the Alaska Department of Health and Social Services, Division of Public Health and Public Health Nursing”.[4] With the support of Senator Stevens, the AFHCAN project received a total funding of USD30.68 million over four years.
Public confidence
In general, public confidence in the project was high: a patient’s satisfaction survey conducted in 2003 showed that 80 percent of patients were satisfied with the service they received through telehealth, and that access to healthcare had increased rapidly.[4] When four beneficiaries were interviewed about the Telehealth Solutions programme, they remarked on the importance of Senator Stevens’ role. “As one interviewee summed it up, ‘Senator Stevens’ involvement – his leadership on the issue, his insistence that the telemedicine systems should be integrated and his appropriations for the equipment and to manage the development’.”[4]Clarity of objectives
The overall objective of the project was to increase both the quality of healthcare and access to medical staff, even in remote areas. There is no official government document stating the policy's precise objective, but that has been the goal ever since the project began. Other important objectives include cost-saving and enhancing the transfer of information between rural clinics and regional healthcare centres. Cost-savings have been achieved by reducing the need for interventions such as flying patients to regional hospitals for treatment.
In January 1999, after a needs assessment, the Alaska Telehealth Advisory commission set out five main policy objectives:
- “Explore and document the potential for and challenges to telehealth development and delivery in Alaska, using the best professional information available
- “Propose a framework for rational development and deployment of statewide capacity for telehealth/telemedicine systems
- “Establish core principles to ensure a coordinated, cost-effective, and integrated approach to telemedicine in Alaska
- “Consider ways to assess effectiveness, efficiency, and the improvement through telemedicine, if any, in equity of access to health services for all Alaskans
- “Recommend a long-term process for addressing issues as they emerge with changing technologies and practice patterns.”[4]
To measure these objectives, subgroups were created that developed metrics to measure their objectives and reported back to the commission (see Measurement below).[4]
Strength of evidence
After numerous conferences and discussions on how to improve ease of access and the quality of healthcare for Alaskans, the NSHC worked with Alascom (an AT&T-owned network provider) to put together a pilot project in one of their villages, using a device called a picture phone. The pilot system, which was called the Alaska Telehealth Testbed Project, enabled users to carry out diagnostic procedures, including consultation with out-of-state specialists.[4]
The pilot was able to demonstrate several benefits of a telemedicine service, such as bringing healthcare services to remote villages using existing low-quality phone lines. It also showed that most of the Community Health Aides who work in the remote centres were able to operate the phone and its diagnostic tools with minimal training. This then informed the further development of the telemedicine cart, which contained a videoconferencing tool producing pictures that could be transmitted through very basic phone lines.[4] Lessons were learned from telehealth programmes elsewhere, including a telemedicine setup in Ontario, Canada, where 2,600 telehealth systems are in use at 1,400 sites.
The success of several clinical telemedicine encounters from the pilot, together with the positive experiences from Ontario, were enough to suggest to other federal health organisations that - with a few enhancements - this technology could be of benefit to remote health providers throughout Alaska. The original plans were expanded and carried forward to Senator Stevens' office with a request for funding to include all the federal healthcare facilities in the state. Today's statewide network of telemedicine computers and diagnostic equipment is a direct result of that determination to improve the delivery of healthcare to remote Alaskan communities.[10] The Alaskan idea of a telemedicine system has now been exported to Greenland and parts of Siberia.
Feasibility
In interviews, key stakeholders identified funding and regulatory issues as an impediment to the further development of telemedicine. While initially the main feasibility issue was the software development cost for the mobile carts, the main concerns for the successful implementation of the policy became the long-term expense, and hence sustainability, of telemedicine. For example, Alaskan providers in the public sector relied heavily on the Universal Services Fund to make the state-of-the-art videoconferencing more affordable. The Fund was established along with the telehealth initiative in 1998 and subsidises telecommunication “to allow more affordable telecommunication rates in rural areas of the state”.[4] Yet, there were concerns about whether or not this funding would be available in the long run.
Even without using videoconferencing, the expense of providing training, infrastructure and maintenance were seen as prohibitive, particularly to healthcare providers in the private sector but also to those in the public sector, because there was a lack of integration between the two.[4] In the AFHCAN's service evaluation, healthcare centres in very remote areas also said that they had not “received enough revenue in the process to maintain the necessary equipment and infrastructure to conduct telemedicine encounters”.[4]
Critical to the success of the AFHCAN project was having sufficient funds and resources to provide training to the hundreds of healthcare workers who would be using the new workstations and kiosks. This was understandably a massive undertaking. Initially, the sum of USD2.35 million was budgeted for training, but it was anticipated that there would be a permanent need for such investment.[4] Continuing the training for providers and the technical assistance for the operation and maintenance of technical equipment, as well as providing constant connectivity, have been major financial and logistic challenges faced by health organisations, in both the public and private sectors.[4]
To ease funding pressures, changes were made to the way telehealth services were reimbursed. Since 1998, this had been done through Medicaid, which was a major funder of medical services in Alaska. Initially, federal Medicaid law did not recognise telemedicine as a distinct service and hence reimbursement was difficult and only given in special cases. Finally, in December 2002, “Medicaid reimbursement for telemedicine claims was authorised for services rendered”.[4] However, even though the FCC provides subsidies for rural healthcare providers to help them fund their bills for connectivity and the internet, the funding has been capped at USD400m a year since the initiative commenced in 1998, and has not been increased since.
Management
Much of the first year of the AFHCAN project was spent in planning and developing the programme, using a steering board and six organised committees, as well as the AFHCAN Project Office (APO) staff. They developed an Operating Plan that “laid out specific roles and responsibilities for committee members, the APO, the AFHCAN Steering Board, and member organisations”.[4] This plan also contained specific progress milestones, including a step-by-step participant action item.
The ANTHC manages the telehealth programme and provides statewide health and information technology services to Alaska Natives and American Indians, in addition to supporting local tribal health organisations.[2] The ANTHC employs 28 staff, who manage the initiative and conduct surveys with local healthcare providers on a regular basis to assess the impact telemedicine is having on patients in remote areas.[9]
Dr Stewart Ferguson, the CIO of the ANTHC, ensures that workflow processes and relationships between medical centres are in place before telehealth is actually applied to patients. “They are constantly working on ‘creating large-scale provider networks to get the full benefit of telehealth investment,' he said, while proposing measures to improve the delivery of telehealth. Especially when it comes to incentivising the permanent use of technology as a part of a doctor's everyday practice, Ferguson sees the need to create a more appropriate reimbursement model that encompasses an ‘all-in-one' fee structure for telehealth consultations.”
Measurement
To evaluate the project's impact and effectiveness, the AFHCAN Project Use & Evaluation Data Report was used, incorporating two primary methods of data collection in its store-and-forward programming.[4]
Health organisation surveys of health providers, business personnel, and technology personnel assessed whether the project had increased the access to healthcare and health information in rural and remote areas and also whether it had improved the quality of care at local village clinics and regional medical centres. Surveys assessed the project's impact on providers' skills and identified sustainability issues.[4]
The main indicators to measure the continuous impact of the policy included the cost-savings on travelling, since critical conditions could be avoided by detecting deteriorating conditions. The AFHCAN also measured how long patients had to wait to see a specialist. This waiting time could be reduced significantly over the course of implementing the Telehealth Solutions programme, especially due to the fact that turnaround times were a lot shorter and most of the patients could be treated within the same day. Between 1991 and 2001, 47 percent of patients had to wait for longer than four months for an appointment. Thanks to the introduction of telemedicine, this number was reduced to 3 percent in the period between 2005 and 2007.
There were six main measures informing the AFHCAN's approach to telemedicine, as developed by researchers from the University of Alaska:
- “Quality of care
- Access to care
- Patient satisfaction
- Continuity of care
- Information transfer
- Cost of care/saving.”[4]
Alignment
Alignment between patients and users in the rural clinics was good, since waiting times for appointments could be reduced and many illnesses could be treated within the same district. According to a summative evaluation of the AFHCAN project, the vast majority of telehealth workers who were introduced to the mobile carts said that the equipment was easy to use and made their work more enjoyable. This proved beneficial in achieving the policy objective of improving Alaskans' healthcare.[4]
However, the interests of the healthcare providers and the funding scheme for telehealth services were misaligned. On the providers' part, reports suggested that the way telehealth has been reimbursed may have been a disincentive to its use. More specifically, there may have been too few financial incentives at the provider level to take extra steps, both medical and administrative, to choose telemedicine as an option for reimbursable healthcare, in spite of its advantages and overall cost-savings to the industry.[4] Telehealth has not been on every practitioner's radar, because there is hardly any reimbursement through Medicaid.
Bibliography
[1] Alaska - Ground Zero for Telehealth Innovation and Deployment, Eric Wicklund, 30 September 2011, Healthcare IT News
http://www.healthcareitnews.com/news/alaska---ground-zero-telehealth-innovation-and-deployment
[2] AK - Regulation - Telemedicine/Telehealth Definition, Center for Connected Health Policy.
http://www.cchpca.org/ak-regulation-telemedicinetelehealth-definition
[3] Telehealth program key to quality healthcare in Alaska, Kristen Lee, TechTarget
https://searchhealthit.techtarget.com/feature/Telehealth-program-key-to-quality-healthcare-in-Alaska
[4] Evolution & Summative Evaluation of the Alaska Federal Health Care Access Network Telemedicine Project, November 2004, University of Alaska Statewide Health Programs and University of Alaska Anchorage Center for Human Development
http://www.akleg.gov/basis/get_documents.asp?session=29&docid=52451
[5] Availability and Deployment of Telemedicine/Telehealth Technologies in Rural Alaska, Burhan Khan et al., December 2012, HHS Public Access Author Manuscritps https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4689206/
[6] Telehealth Improves Access and Quality of Care for Alaska Natives, Innovations Exchange Team, 22 May 2013, Agency for Healthcare Research and Quality
https://innovations.ahrq.gov/perspectives/telehealth-improves-access-and-quality-care-alaska-natives
[7] Alaska Enacts New Telemedicine Law: What Providers Should Know, Nathaniel M. Lacktman and Thomas B. Ferrante, 13 July 2016, Foley & Lardner LLP
[8] Commentary: FCC is committed to rural telemedicine in Alaska, Aji Pai, 20 June 2018, Alaska Journal of Commerce
[9] The AFHCAN Telehealth Program, Stewart Ferguson and John Kokesh, Alaska Native Tribal Health Consortium
[10] The Ultimate Telemedicine Guide - What Is Telemedicine?, 25 May 2018, eVist
https://evisit.com/resources/what-is-telemedicine/
[11] The Evolution of Telehealth: Where Have We Been and Where Are We Going?, Thomas S. Nesbitt, 2012, The Role of Telehealth in an Evolving Health Care Environment: Workshop Summary, the National Academy of Sciences.
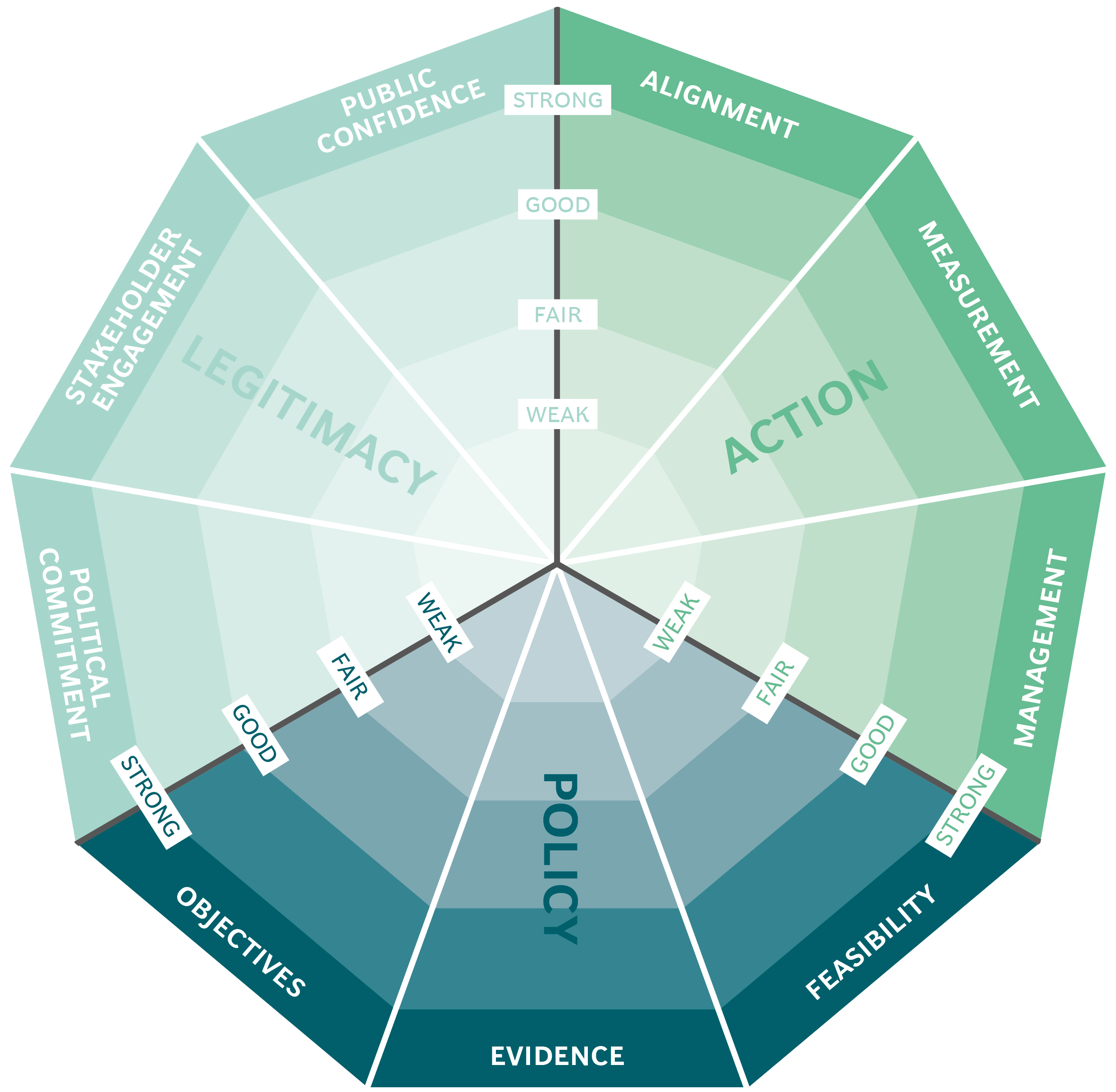
The Public Impact Fundamentals - A framework for successful policy
This case study has been assessed using the Public Impact Fundamentals, a simple framework and practical tool to help you assess your public policies and ensure the three fundamentals - Legitimacy, Policy and Action are embedded in them.
Learn more about the Fundamentals and how you can use them to access your own policies and initiatives.
You may also be interested in...


Mexico City's ProAire programme

National portal for government services and Information: gob.mx

The eco-friendly façade of the Manuel Gea González Hospital tower in Mexico City

Organ Donations in Iran
